Here’s everything you need to know about the neurodegenerative disease amyotrophic lateral sclerosis.
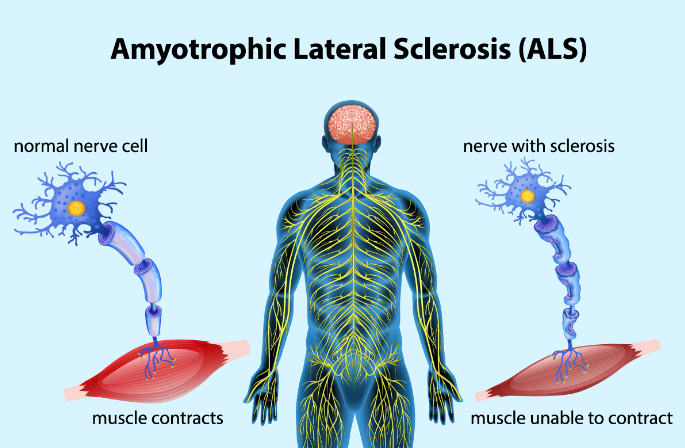
Amyotrophic lateral sclerosis, also known as ALS, is a neurodegenerative disease that worsens over time, impairing the ability of certain nerve cells to perform their intended functions. Amyotrophic Lateral Sclerosis is more common than you may imagine, and it’s also referred to as Lou Gehrig’s disease after the famous baseball player. Author and theoretical physicist Stephen Hawking is another well-known figure whose struggle with Amyotrophic Lateral Sclerosis raised awareness of the illness.
According to Dr. Sabrina Paganoni, a physician-scientist at the Sean M. Healey & AMG Center for ALS at Massachusetts General Hospital in Boston, the lifetime risk of developing ALS is approximately 1 in 400 for women and 1 in 300 for men. The ALS Association estimates that 16,000 Americans are living with Amyotrophic Lateral Sclerosis at any given time.
Also read-Multiple Sclerosis : A Patient’s Guide To Multiple Sclerosis And Its Symptoms
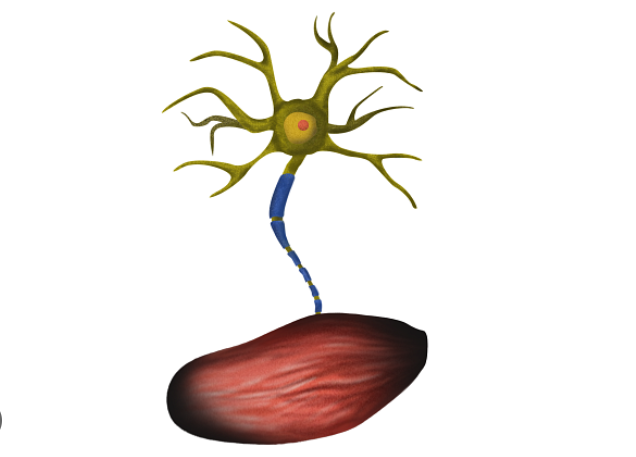
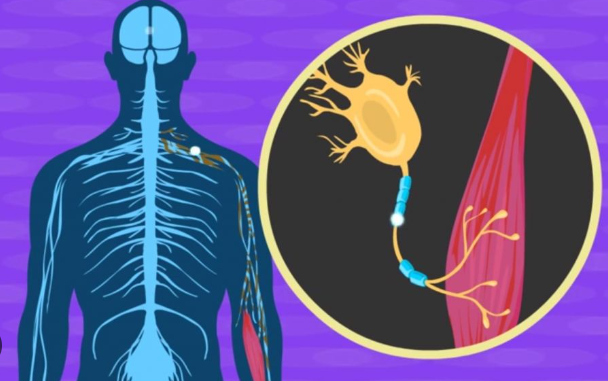
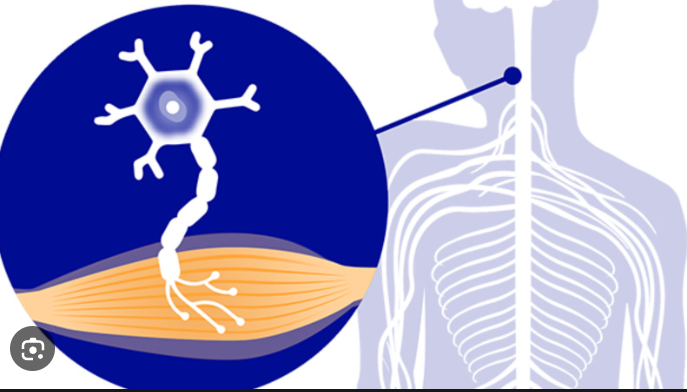
Parkinson’s disease and Alzheimer’s disease are two other instances of neurodegenerative diseases. The loss of muscle mass is referred to as amyotrophic. Neural cells, or neurons, are found in our brain and spinal cord. ALS impairs the normal function of those neurons, making it impossible to produce muscle movement. These muscles eventually lose their ability to function due to their weakness.
“Anything that moves because of muscle or is composed of muscle can be affected,” states Kuldip Dave, the ALS Association’s vice president for research. “Eventually you lose your ability to speak, move, and breathe.”
Causes and risk factors Amyotrophic Lateral Sclerosis
In 90% to 95% of ALS cases, the exact cause of ALS is unknown. “If we did know what caused it, it would make it easier to target it,” Dave says. Because the cause is typically unknown, there is also no way to actively prevent the disease. ALS without a clear cause is referred to as sporadic.
About 5% to 10% of ALS cases are caused by gene mutations. This is known as a familial cause. Some, but not all, of the genes associated with ALS have been identified.
At this point, researchers think it could be a combination of environmental factors, genetic traits, exposures, and lifestyles that cause the disease.
There are two known risk factors for ALS:
- Being older. The average age at which Amyotrophic Lateral Sclerosis is typically diagnosed is 60. Those with ALS in the family are typically diagnosed at age 50, according to Paganoni. However, ALS can strike at any age.
- Being male. Men are 1.56 times more likely to get Amyotrophic Lateral Sclerosis than women, according to the ALS Association.
Studies have discovered links between ALS and additional variables. This indicates a correlation but not a cause-and-effect relationship. As an illustration, according to certain research, veterans of the armed forces may have a 1.5–2 fold increased risk of developing Amyotrophic Lateral Sclerosis, notes Dr. Matthew B. Harms, medical adviser to the MDA and associate professor of neurology at Columbia University’s neurology department in New York City. There could be a link between exposure to toxins and intense physical activity. As a disease related to military service, ALS is recognized by the US Department of Veterans Affairs. This implies that military service may contribute to it or make it worse.
Symptoms
The symptoms of amyotrophic lateral sclerosis can vary widely. One person initially may have trouble grasping a pen and holding a coffee cup but have no trouble speaking, Dave says. Yet another person may have trouble speaking but can still easily hold a pen or cup.

Symptoms may start differently in each person, but they tend to be fast moving and progress until they are severe – for example, having trouble breathing and requiring a respirator.
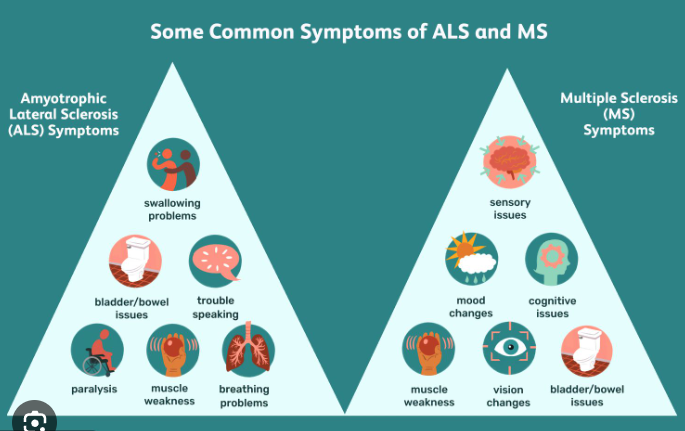
Here are some of the common symptoms associated with ALS:
- Muscle twitches (also called fasciculations) and spasms This symptom is common in the early stages of Amyotrophic Lateral Sclerosis.
- Tripping or stumbling.
- Weak arm or leg muscles. This usually starts in one arm or leg and then spreads to other body parts. As muscles are less used, joints become rigid, painful and sometimes deformed, Harms says.
- Hand weakness. Tasks like using buttons or zippers, handling coins, turning a key in a lock or writing become difficult.
- Inappropriate and uncontrollable laughing or crying. This is also called pseudobulbar affect.
- Impaired decision-making and other declining cognitive skills This occurs in as many as 15% of people with Amyotrophic Lateral Sclerosis, Harms says.
- Trouble speaking or swallowing.
- Fatigue.
- Trouble breathing.
Diagnosis
There isn’t a particular test to identify. Amyotrophic Lateral Sclerosis Doctors frequently utilize tests to help rule out conditions like multiple sclerosis and other illnesses with symptoms that are similar to one another. According to Paganoni, the diagnosis of ALS typically takes a year because the disease is difficult to identify. Due to the lack of a specific test, people seeking a diagnosis for ALS frequently consult with multiple specialists before a diagnosis is made.
The following tests, in addition to a clinical examination, are used to diagnose ALS:
- Electromyography. This test measures how well the nerves and muscles are working. It can help measure how much nerves and muscles have weakened.
- Magnetic resonance imaging This imaging test is used to take images of the brain and spinal cord. An MRI can help rule out the diagnosis of conditions other than amyotrophic lateral sclerosis.
- Blood and urine tests. Again, these may be used to help rule out other diseases. Currently, there’s no biomarker that can be identified in a blood test to show a person has ALS.
Although it’s not always used, genetic testing plays a part in ALS cases. Although most of the genes that cause ALS are testable, Paganoni notes that not all of the genes are currently understood to be involved. Based on that family history, it may make sense to move forward with genetic testing if someone has a family member who has ALS, she says. This is due to the fact that, according to the ALS Association, an individual who carries an ALS gene mutation has a 50% chance of passing the gene on to their offspring. Nevertheless, an individual does not automatically get ALS just because they have a gene mutation.
As the illness worsens, more testing might be required, according to Cardiel. This may consist of:
- A pulmonary assessment is needed to determine lung capacity.
- A swallow test to determine whether dietary modifications are necessary. In order to guarantee they get enough food, people with ALS eventually require a feeding tube.
- A sleep study to find out if someone needs more assistance to have a restful night’s sleep.
Treatment
Although there is no cure for ALS, there are some medications that can slow the progress of the disease.
- It is believed that riluzole lessens nerve cell damage. It doesn’t undo damage already done; it might extend survival by several months. Fatigue, nausea, and potential liver damage are among the side effects of riluzole.
- Edaravone is an intravenous medication that can reduce the rate at which bodily functions deteriorate by eliminating free radicals, which can harm or even kill cells. In one clinical trial, the drug’s IV treatment group showed a 33% reduction in physical function decline when compared to the placebo group.
One medication called Nuedexta, which combines quinidine and dextromethorphan, is used to help manage pseudobulbar affect, which is involuntary laughing or crying. Patients with dementia and multiple sclerosis, among other neurodegenerative conditions, are also treated with this medication.
Other medications are administered to treat symptoms arising from conditions that commonly affect individuals with ALS, such as:
- Depression and anxiety
- Drooling.
- Pain.
- Inability to sleep or problems getting quality sleep
In addition to medications and getting help from doctors and nurses, there are many other health professionals involved in the care of someone who has ALS. “Because ALS is so complex, care needs to be comprehensive,” Paganoni says. Here are some of those professionals and how they help:
- Equipment specialists help demonstrate how to use equipment to assist in mobility.
- Physical therapists help restore and maintain muscle strength and function.
- Occupational therapists can help those with ALS conserve energy and still remain mobile. They do this by showing those with ALS how to modify their activities of daily living.
- Respiratory therapists can show how to use breathing-related devices.
- Registered dietitians assist with nutritional needs as swallowing becomes more difficult.
- Speech therapists help to make speech more understandable.
Around the U.S., there are multidisciplinary care centers where the various professionals who work with ALS can be seen at the same place.
Additionally, there’s technology that can help people with ALS. “Computer-based speech synthesizers that use eye-tracking technology can help with nonverbal communications, and voice banking allows patients to store their own voice for future use,” Harms says.
Caregivers also help those with ALS manage their declining mobility. Falling, difficulty walking, and fatigue commonly occur, the MDA reports. For this reason, many assistive devices are part of the care of a person with ALS, including:
- Canes.
- A power wheelchair.
- A walker.
- Supportive braces.
Also read-Brain-Heart Coherence Techniques: Balancing Mind And Body
images source: Google
Disclaimer: The opinions and suggestions expressed in this article are solely those of the individual analysts. These are not the opinions of HNN. For more, please consult with your doctor.