Learn about the symptoms, causes, and life expectancy of vascular dementia.
Vascular dementia is not as well-known as Alzheimer’s disease, but perhaps it ought to be, given how devastating both conditions are. The fact that vascular dementia is more preventable than the other two brain disorders may be the most significant distinction between them. Here’s why you should start looking into it and acting on it right away.
Vascular dementia claimed the lives of over 16,000 Americans in 2017, the Centers for Disease Control and Prevention report. It is common to have vascular dementia. An Alzheimer’s Association report from 2018 estimated that 5.7 million Americans had Alzheimer’s dementia. Pure Alzheimer’s disease would make up roughly 60% of a pie chart comparing different forms of dementia, according to Caroline Harada, a geriatrician with the University of Alabama at Birmingham.Pure vascular dementia would represent about 15%. Another 15% to 20% would be people who have a combination of Alzheimer’s and vascular dementia.
Also read-Dementia : A Patient’s Guide To Dementia And Its Symptoms

Types of vascular dementia
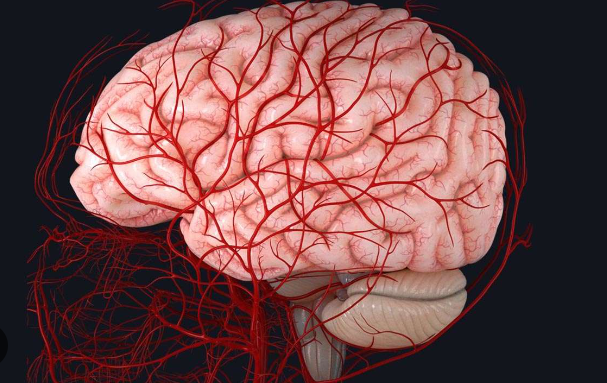
Alzheimer’s disease, Lewy body, frontotemporal, and vascular dementia are among the various forms of dementia that fall under the general term dementia. Vascular dementia is characterized by a reduction in blood flow to the brain.
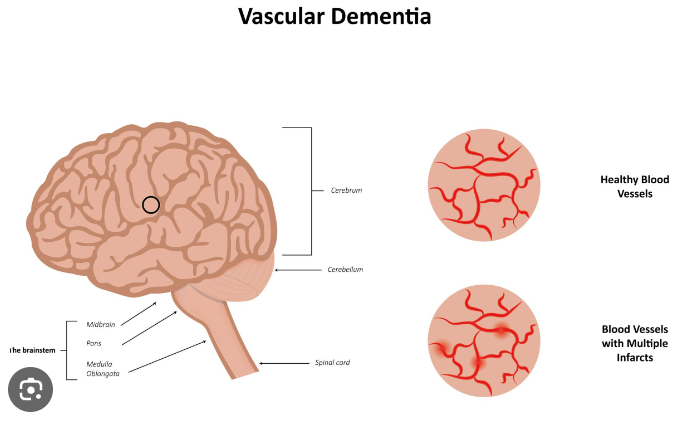
“This particular form is caused by blockages of the blood vessels that feed the brain,” Harada clarifies. According to her explanation, a blockage could be large enough to result in one or more strokes, and dementia could strike right away. On the other hand, small-vessel disease affects the tiny capillaries that supply the brain cells. She asserts that “there is never one big, dramatic moment in the absence of a stroke.” The brain damage that leads to dementia is more like a slow, steady burn.”
Symptoms
Vascular dementia’s course is often unpredictable.The symptoms can slowly creep up on people, not becoming obvious for many years. Once diagnosed, the condition can feel like a roller-coaster ride. “Vascular dementia seems to fluctuate a bit more than nonvascular dementia,” says Dr. Bruce Miller, director of the Memory and Aging Center at the University of California–San Francisco. “There are, in many cases, halting improvements for a short period of time, then a second stroke happens and worsens again. It’s a much more rocky and up-and-down kind of course.”

Alzheimer’s and vascular dementia appear to affect different types of brain function. Alzheimer’s tends to erode a person’s memory and word-finding ability. By contrast, vascular dementia is more likely to affect executive function. “Typically, what tends to happen first is difficulty with attention span and difficulty with the speed at which you process information,” Harada says. “And difficulty with executive function—judgment, reasoning, complex problem-solving—all those tasks. Those are a lot more subtle, and it can take families longer to clue in that there’s really a problem.”
The symptoms of vascular dementia can differ greatly, according to the Alzheimer’s Association, “depending on the part of the brain affected and the severity of the blood vessel damage.” Depending on which specific brain regions have less blood flow, memory loss may or may not be a serious symptom.”
A major stroke may cause symptoms to become more noticeable. These could consist of:
- Confusion.
- Disorientation.
- Trouble speaking or understanding speech.
- Vision loss.
Risk factors
Medical conditions and health behaviors that put people at risk for stroke and heart disease also make them more vulnerable to vascular dementia.
Cardiovascular risk factors include:
- Smoking.
- Hypertension.
- Diabetes.
- Lack of exercise
- High cholesterol.
It’s also known that people with atrial fibrillation, or AFib, are more likely to develop vascular dementia than the general population. The connection: Having AFib puts you at much higher risk for stroke, thus raising your risk for dementia, Harada explains.
Diagnosis
Wellness exams.
Medicare pays for older adults’ yearly wellness visits, which ought to involve a cognitive evaluation. Signs of cognitive impairment can be identified with a medical history and with quick tests such as the Montreal Cognitive Assessment, or MoCA. “These wellness exams are when the risk factors for vascular dementia are picked up,” says Miller. “When health practitioners do cognitive screening, it’s going to show there are subtle cognitive changes.” Blood tests may be ordered by geriatricians or primary care physicians in order to rule out other conditions. MRIs and other brain imaging tests may be performed on patients. “In some cases, in the course of an evaluation, an MRI will show extensive vascular changes,” says Miller. To determine the kind and stage of dementia, a neurologist can perform additional testing.
Early detection.
According to Miller, vascular dementia is an “epidemic.” “It’s usually silent. Depending on the cause, more damage can frequently be avoided if it is identified. The likelihood of a successful outcome increases the earlier we enter someone’s path. And there are undoubtedly a lot of positive results for people. It must be early, though. It is not possible that it occurs after several avoidable strokes. It truly is a tragedy for humankind.” According to him, family members should consult a specialist when a person’s heart or brain blood vessels are in danger.
Treatment
Because the disease process, or pathophysiology, is so different for Alzheimer’s and vascular dementia, treatment is different, too. Alzheimer’s drugs don’t work as well for vascular dementia.”We have some drugs that work for Alzheimer’s, such as cholinesterase inhibitors and NMDA antagonists like Memantine,” Harada says. “Those drugs do not seem to work as well for patients who have vascular dementia.” Cholinesterase inhibitor drugs include Aricept, Razadyne, and Exelon.
Quality of life is a major goal.Once someone is diagnosed with vascular dementia, “focusing that time on maintaining a really good quality of life and making sure that the person is well-cared for and surrounded by people who love them” becomes the care priority, Harada says. “And trying to be as active as they can, doing things they enjoy.”
Vascular dementia is tied to a shorter life expectancy.On average, an individual with Alzheimer’s disease lives four to eight years after being diagnosed, but can live as long as 20 years, according to the Alzheimer’s Association. In contrast, people with vascular dementia live about five years after symptoms start, according to the association. Oftentimes, a stroke or heart attack is the cause of death.
Also read-Dementia : A Patient’s Guide To Dementia And Its Symptoms
images source: Google
Disclaimer: The opinions and suggestions expressed in this article are solely those of the individual analysts. These are not the opinions of HNN. For more, please consult with your doctor.




































