Know the basics of symptoms, diagnosis, and treatment to help you battle Crohn’s disease.
Everybody has occasionally had upset stomachs, perhaps from eating a bit too much junk food, and as a result, they have suffered cramps, bloating, nausea, pain, or gas. These types of episodes usually last a few days at most. However, some people experience similar episodes of upset stomach that last a lifetime; in these cases, they might have Crohn’s disease, an autoimmune condition.
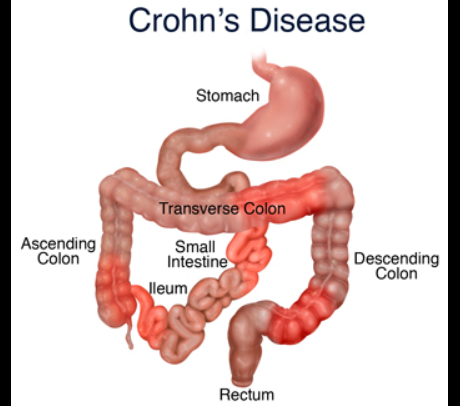
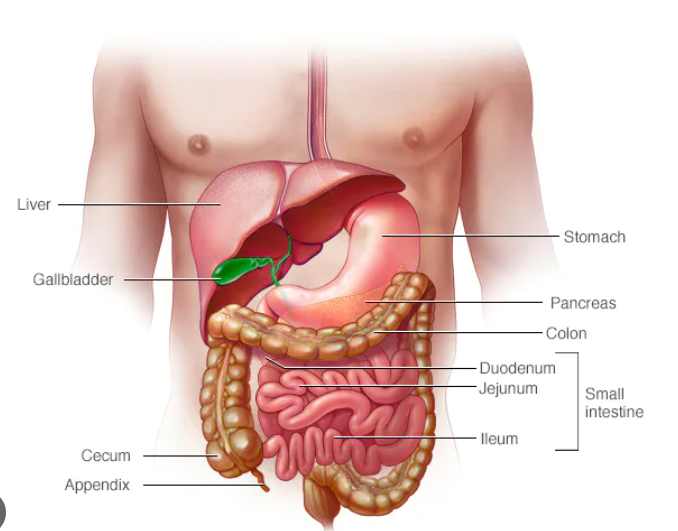
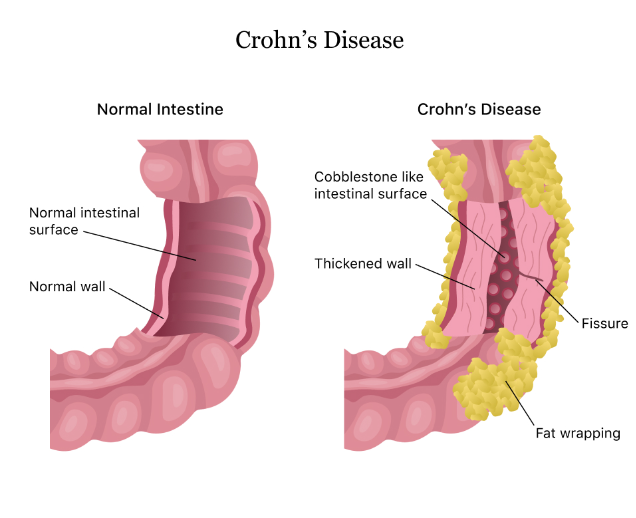
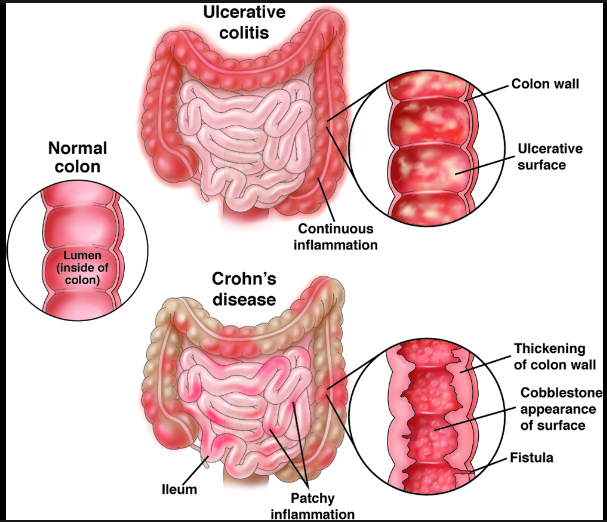
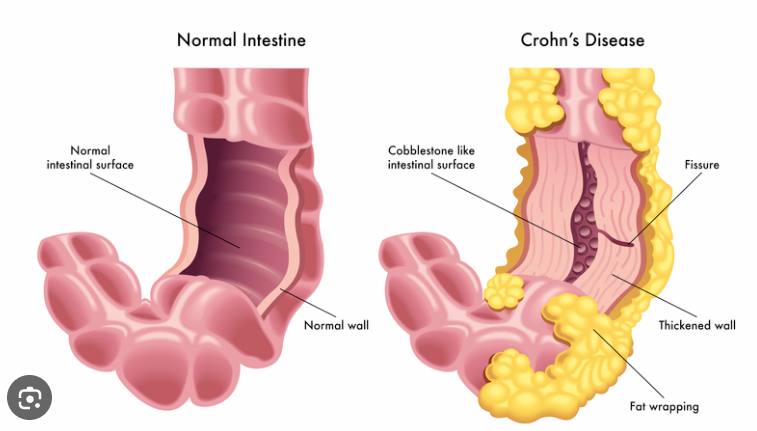
The gastrointestinal tract’s lining becomes inflamed as a result of Crohn’s disease, according to Dr. Miguel Regueiro, the chair of the gastroenterology, hepatology, and nutrition department at Cleveland Clinic in Ohio. It is frequently included in the general category of inflammatory bowel disease, along with another illness known as ulcerative colitis.
Also read-Osteoporosis : A Patient’s Guide to Osteoporosis
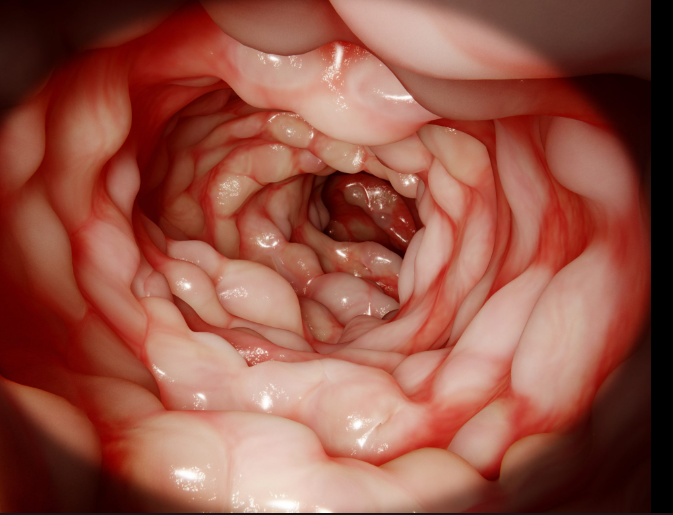
According to Regueiro, Crohn’s disease can develop anywhere in the digestive tract, from the mouth to the rectum or the anus. Anywhere along the digestive tract, the inflammation can manifest itself patchily and isn’t always constant. In contrast, only the large intestine and the rectum are inflamed in ulcerative colitis cases. “The small intestine is the most common site of Crohn’s disease appearance.”
Although Crohn’s and colitis are often talked about together, “Crohn’s disease should not be confused with ulcerative colitis, which is another type of IBD,” says Dr. Niket Sonpal, a New York-based gastroenterologist, internist, and adjunct professor at Touro College in New York. “The disease consists of inflammation throughout the gastrointestinal tract and reactions to different types of foods and substances.”
Crohn’s is an autoimmune disorder in which the body’s immune system, which is designed to protect the body from foreign infectious agents, gets confused and begins attacking the body’s own cells. “It’s an immune-mediated disease, meaning that our own body’s immune system begins to attack the intestine to cause this inflammation,” Regueiro says.
Causes of crohn’s disease
Crohn’s disease was first described in the 1930s, Sonpal says. “Early on, we thought that it was caused by diet and stress. But as more research and observation have taken place in the nine decades since, doctors are still not able to pinpoint the exact cause of this disease. We do know, however, that diet and stress can exacerbate the symptoms of the disease.”
Regueiro says “current research has demonstrated that it is likely a variety of factors,” which may include:
- Environmental influences.
- Genetics.
- Diet.
“There is likely some environmental influences on the gastrointestinal tract,” he says. “We don’t know if it’s diet or something in the environment that leads to this trigger for the immune system to begin to attack itself,” but it seems likely that genetics also plays a role, given that some people develop the disease while others don’t. However, Regueiro says many gastroenterologists believe that environment is probably the biggest factor “because the microbiome and bacteria in the gut probably play a role, but we clearly know the immune system is attacking an otherwise normal intestine to cause these ulcers and this inflammation.”
Signs and symptoms
Per Regueiro, “the most typical signs of Crohn’s disease are typically diarrhea and abdominal pain.” But those are the most typical symptoms. There are numerous ways the illness can manifest itself.
Sonpal continues, saying that “each patient experiences the disease in a unique way. They may experience different foods that cause different amounts of pain, and the degree of other symptoms like diarrhea, cramping in the abdomen, and bleeding in the rectal area may also vary.
According to the Mayo Clinic, common Crohn’s disease symptoms include:
- Diarrhea.
- Abdominal pain and cramping
- Fever.
- Fatigue.
- Bloody stools.
- Unintended weight loss and reduced appetite.
- Sores or lesions in the mouth
- Pain and inflammation around the anus
- Inflammation of the skin, eyes, joints, liver, or bile ducts
Risk factors
Although Crohn’s disease can be diagnosed in anyone at any age, it tends to be more common in adults. The Centers for Disease Control and Prevention report that an estimated 3 million adults in America—about 1.3 percent of adults—had either Crohn’s disease or ulcerative colitis. Sonpal notes that studies vary in their estimation of the number of people in the U.S. with Crohn’s but it’s likely anywhere from 700,000 to 1.5 million.
The Mayo Clinic reports that some risk factors appear to be associated with a higher chance of developing Crohn’s disease, including:
- Age. Most people are diagnosed with Crohn’s disease around the time they’re 30 years old.
- Sex. “In terms of population studies, research shows that women are more susceptible to Crohn’s disease than men,” Sonpal says, “though men can still be affected by the disease.”
- Ethnicity. “Though people of all ethnicities can be and are affected by Crohn’s, studies show that Caucasian people are diagnosed at a higher rate, followed by African Americans, whose diagnosis rate has been on the rise, according to recent information gathered on the disease,” Sonpal says.
- Family history. If your parent, sibling, or child has Crohn’s disease, you’re more likely to develop it, too.
- Cigarette smoking. Smoking has been associated with the development of Crohn’s disease and is the most easily controlled risk factor.
- Nonsteroidal anti-inflammatory medication use. Although medications that include over-the-counter painkillers such as ibuprofen and naproxen sodium don’t directly cause Crohn’s disease, they can lead to inflammation of the bowel that can exacerbate a case of Crohn’s.
- Geography. People living in urban or industrialized nations are more likely to develop Crohn’s, suggesting that environmental or dietary factors may be causing that increased incidence.
People with Crohn’s and colitis are also more likely to have other chronic health conditions as well, including:
- Cardiovascular disease.
- Respiratory disease.
- Cancer.
- Arthritis.
- Kidney disease.
- Liver disease.
Diagnosis
The Crohn’s and Colitis Foundation reports that “a variety of tests are used to diagnose and monitor Crohn’s disease and ulcerative colitis, the two main types of inflammatory bowel disease. Procedures range from simple blood tests to barium X-rays and colonoscopy, which require preparation the day before the tests. A proper diagnosis of IBD involves determining the disease type (Crohn’s disease or ulcerative colitis), the extent and severity of the disease, and any related complications.”
Treatment
“The most common treatment approach is some type of medication,” Regueiro says. Although there is still no cure, he says the medications that are available now are much better than they were even just 10 years ago. “We have a lot of new medicines that are targeted at parts of the immune system that control inflammation. These are what we call biologic medicines or biologically active medicines,” and they can bring down the level of inflammation in the body and reduce your experience of symptoms.
“Depending on your case, a doctor might treat your disease with anti-inflammatory medication to reduce inflammation, steroids, immunosuppressant medication to reduce your body’s response to attacking cells in the GI tract and sometimes antibiotics to stop any harmful bacteria from growing,” Sonpal says.
Also read-Fibromyalgia : A Patient’s Guide to Fibromyalgia And Its Symptoms
images source: Google
Disclaimer: The opinions and suggestions expressed in this article are solely those of the individual analysts. These are not the opinions of HNN. For more, please consult with your doctor.




































