End-stage renal failure, dialysis, or a kidney transplant can often add years to your life.
A diagnosis of end-stage renal failure comes as a shock to a lot of people. The final stage of chronic kidney disease, often known as end-stage renal disease, end-stage kidney disease, or renal failure, is an incurable condition that progresses silently with few to no symptoms. Nearly 40% of patients suffering from end-stage renal failure have never received any kind of nephrology care before. According to Dr. Anjay Rastogi, clinical chief of nephrology at UCLA Health, “it might not have been discovered early enough, or you might have been reluctant to follow up because you felt fine and thought, ‘Why do I need to take medication when I have no symptoms?'”
But when kidney disease worsens, end-stage renal failure can strike, bringing with it the devastating realization that you will either need a kidney transplant or dialysis to survive and that your chances of survival are now very slim. It’s a concerning and dangerous condition. You consider the death rate from cancer to be among the lowest in the world. However, kidney failure-related deaths can occasionally be higher, according to Dr. Richard Fatica, vice chair of the Cleveland Clinic’s nephrology and hypertension department.
Also read-Renal Failure : A Patient’s Guide To End-Stage Renal Failure And Its Symptoms
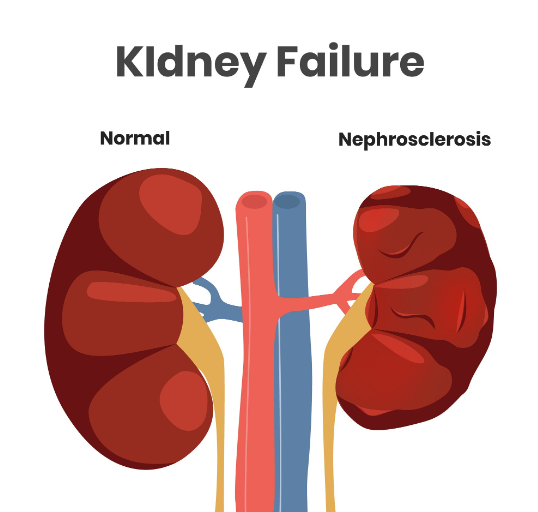
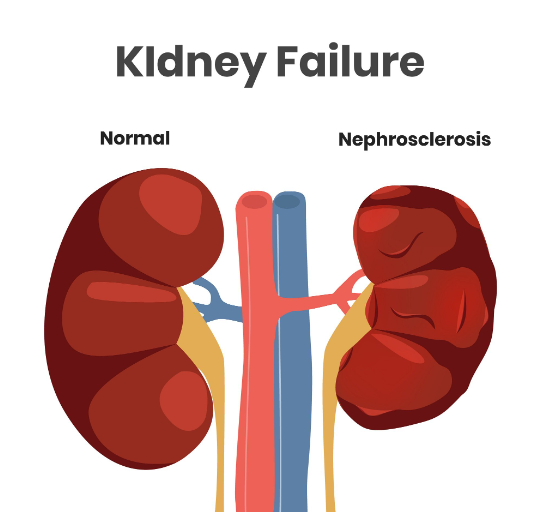
Causes of renal failure
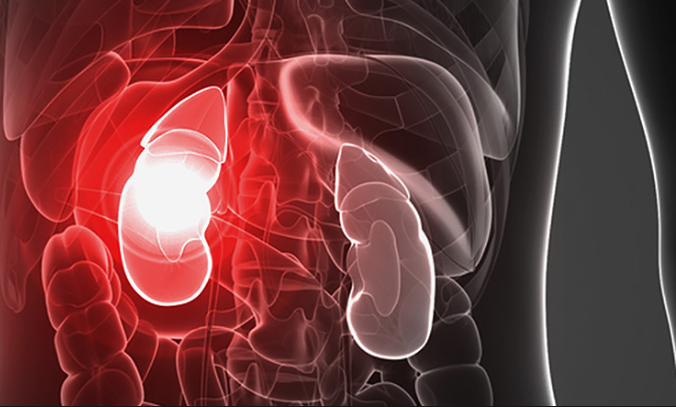
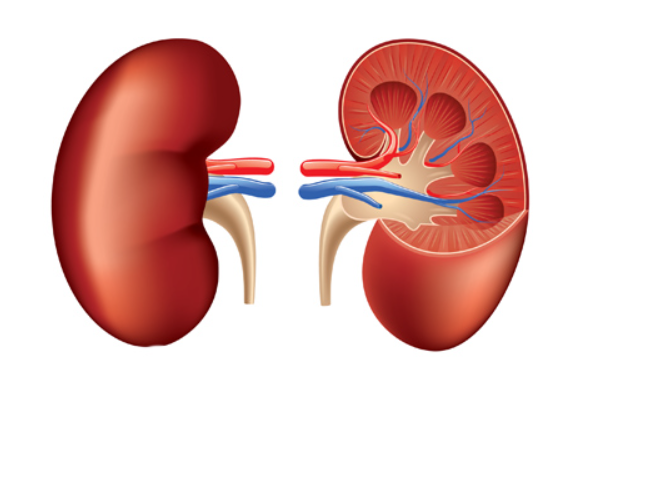
End-stage renal failure results from damage to the kidneys, two bean-shaped organs on either side of the spine. The kidneys have crucial jobs:
- They make the blood clean. A kidney’s glomeruli, which are microscopic filters that eliminate chemicals, toxins, and excess fluid that build up as blood flows through a huge network of blood vessels, number about a million per kidney. Urine excretes the debris.
- In addition, the kidneys regulate hormones, chemicals, and minerals that support bone health, blood pressure regulation, and red blood cell production.
Symptoms of renal failure
When kidney damage first occurs, you might not experience any symptoms at all. Alternatively, you might have vague symptoms (difficulty falling asleep, fatigue, foggy thinking) that you attribute to other disorders that have already been diagnosed, like diabetes.
But the kidneys will cease to function effectively as kidney disease progresses to end-stage renal failure. Extra fluid and waste will consequently build up in your body. At that point, certain symptoms might stand out more, like:
- Changes in urination (much less urine).
- Shortness of breath (from fluid buildup in the lungs).
- Swollen feet and ankles (from fluid buildup).
- Unexplained itching.
- Nausea and vomiting
- Unexplained weight loss.
- Chest pain (from fluid buildup near the heart).
- Muscle cramps and twitching.
- Reduced appetite.
The diagnosis of renal failure
Your doctor may request a straightforward blood and urine test if they think you might have kidney disease. Your doctor might refer you to a nephrologist, a specialist in kidney care, if the results show abnormalities.
Your medical history and any additional health issues you may have, such as diabetes or cardiovascular disease, will be discussed with the specialist. The medical history of your family is also very significant. You can expect a physical exam that includes a blood pressure measurement. Your doctor may also order tests to measure your kidney function and look at their structure. These tests can include:
- Blood tests to look for waste products (such as creatinine, produced by the muscles) no longer being excreted in the urine.
- Urine tests are used to check for levels of protein being excreted. High protein levels can be a sign of reduced kidney function.
- Imaging tests such as CT scans, MRIs, or ultrasounds look for changes in your kidney structure.
- Biopsies (removing samples of kidney tissue) are needed to determine the type of kidney disease you have.
Treatment of renal failure
We don’t yet have a way to cure end-stage renal failure. The three main approaches to treatment include:
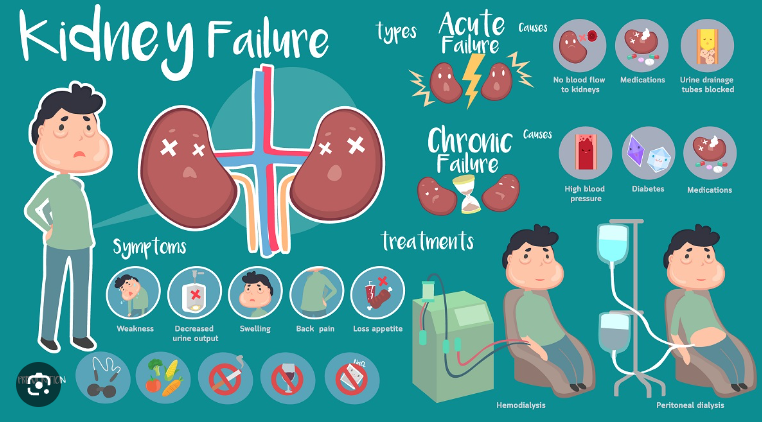
- Dialysis. Dialysis helps remove toxins and extra fluid from your blood. You might have hemodialysis and be hooked up to a machine that runs your blood through a filter and returns it to your body. Or you might have peritoneal dialysis, which fills the space around your abdominal organs (the peritoneum) with a fluid that flushes toxins and extra fluid from the peritoneal lining. The fluid is drained and then replaced with clean fluid. You’ll need dialysis several times a week. “Although survival on dialysis has improved, patients on average live about a quarter of the expected life of someone without kidney disease,” Fatica says. “So if you’re 60 and you’d normally live to 80, you might be expected to live five years on dialysis.”
- A kidney transplant. “Transplantation approximately triples life expectancy compared to being on dialysis. So if dialysis would extend your life another five years, a kidney transplant could extend your life another 15 years,” Fatica says. “Additionally, if a kidney transplant fails, patients can most often go back to dialysis.” But not everyone is a candidate for a kidney transplant, and about 95,000 people in the U.S. are on a waiting list for a kidney. “In most urban areas, there’s a five-year waiting list for a deceased donor. You can get one faster if you have a living donor,” Charytan says. In 2018, about 21,000 people in the U.S. received kidneys from deceased and living donors.
- Conservative management. Sometimes patients forego dialysis or a transplant. The approach involves managing symptoms with medications so patients feel better. “This is typically for people who have a shorter life expectancy and don’t want a poor quality of life on dialysis. You might be able to manage the disease for a year or longer. If it’s more advanced, it might be less,” Rastogi says.
Also read-Coronary Artery Disease : A Patient’s Guide To Coronary Artery Disease And Its Symptoms
images source: Google
Disclaimer: The opinions and suggestions expressed in this article are solely those of the individual analysts. These are not the opinions of HNN. For more, please consult with your doctor.




































