According to the data, the likelihood of white women being admitted to an intensive care unit during their hospital stay for childbirth is the lowest.
Women of color, older mothers, and women giving childbirth to more than one baby are among those most likely to require intensive care during a delivery hospitalization in the U.S., new research indicates.
“Awareness of the demographic characteristics and medical factors that place mothers at higher risk of ICU admission may help inform efforts to ensure that pregnant women have access to the appropriate level of specialized perinatal care,” says a study released Thursday by the Centers for Disease Control and Prevention’s National Center for Health Statistics.

Reports on hospitalizations for childbirth
The overall admission rate to an intensive care unit for hospitalized mothers delivering live-born infants was 1.8 per 1,000 live births from 2020 to 2022, according to a study released Thursday by the Centers for Disease Control and Prevention’s National Center for Health Statistics. That amounts to an average of 6,634 admissions per year.

Childbirth
Researchers found significantly higher ICU admission rates among mothers from racial and ethnic minority populations who were hospitalized for a delivery compared with white women. Rates were 2.7 per 1,000 live births among American Indian and Alaska Native women and 2.6 per 1,000 among black women, for instance, with the rate among white women at 1.5 per 1,000.

Childbirth
Study on the reports
The study also found the risk of needing ICU admission increased with a mother’s age: women younger than 25 had the lowest ICU admission rate at 1.4 per 1,000 live births, while mothers 45 and older had the highest at 6.5 per 1,000. ICU admission rates rose significantly between age groups, with a 71% increase between rates for mothers 40 to 44 years old and those 45 and up.

Childbirth
Though researchers called ICU admission during hospitalization for a delivery “a relatively rare event,” they stressed that “the risk of severe morbidity and mortality is high among mothers” when such an admission is necessary. “Awareness of the demographic characteristics and medical factors that place mothers at higher risk of ICU admission may help inform efforts to ensure that pregnant women have access to the appropriate level of specialized perinatal care,” the study says.

Childbirth
Reports on the the risk of needing ICU care
The risk of needing ICU care generally increased depending on how many other children a mother had previously delivered, with the rate of admission nearly twice as high among mothers experiencing at least their sixth live birth than among mothers experiencing their first live birth, at 3.5 per 1,000 vs. 1.7 per 1,000.

Childbirth
Mothers giving birth to multiple babies were also at higher risk, with the ICU admission rate among women having twins at 5.3 per 1,000 and the rate among those having triplets or more at 11.5 per 1,000, compared with 1.7 per 1,000 among mothers delivering a single child.

Childbirth
ICU rates during delivery hospitalization, by plurality
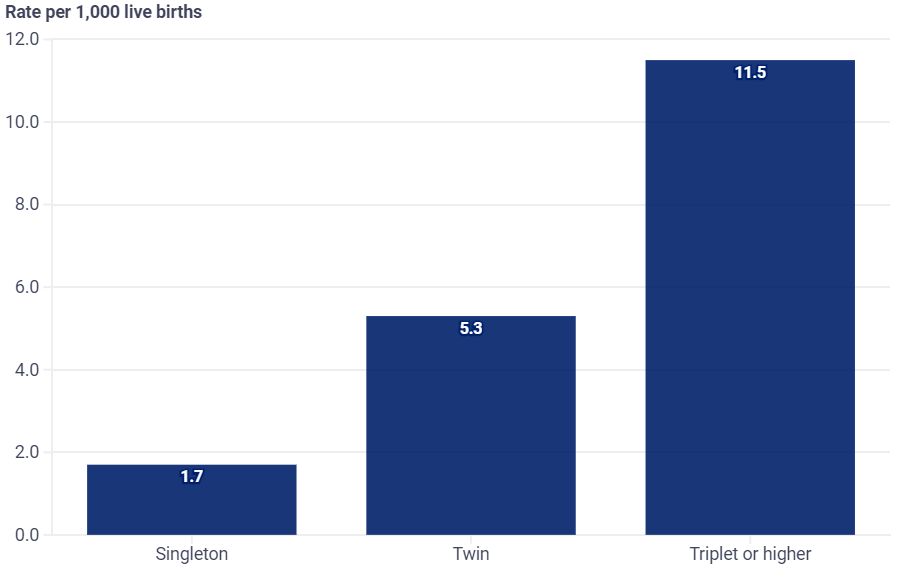
Source: National Center for Health Statistics. Rates above reflect intensive care unit admission rates of mothers during hospitalization for delivery of a live-born infant per 1,000 live births.
The United States continues to struggle with a maternal mortality crisis marked by glaring racial and ethnic disparities and a rate of maternal death that has significantly exceeded the rates of other peer nations. This new study and its demographic data are being released at this time. Maternal mortality rates in the United States in 2021 were 32.9 deaths per 100,000 live births; black women had a rate of almost 70 per 100,000, compared to 26.6 and 28.0 per 100,000 for white and Hispanic women, respectively. Older women also had a higher rate of maternal death; for example, the rate for women over 40 (138.5) was almost 600% higher than the rate for women under 25 (20.4).

Childbirth
Risk factors
And while identifying risk factors is important, Lampley says narrowing disparities in maternal health outcomes for women of color also requires health care providers to listen to their patients when they express concerns about how they are feeling and to be more conscious about addressing issues as they arise. “When patients come into the environment, are their concerns recognized, and are they being treated in the same careful manner such that the alert is raised in an appropriate fashion?” Lampley says. “How the health care system responds to patients of color and also the higher prevalence of underlying conditions in communities of need—those two things, I think, impact these issues.”

Childbirth
Also read-Pneumonia : A Patient’s Guide To Pneumonia And Its Symptoms
images source: Google
Disclaimer: The opinions and suggestions expressed in this article are solely those of the individual analysts. These are not the opinions of HNN. For more, please consult with your doctor




































