Your guide to the causes, symptoms, treatments, and more of tuberculosis.
There was once a widespread fear of the infectious disease; tuberculosis was once referred to as “consumption” because the afflicted person was completely consumed by it. Today, most cases of tuberculosis (TB) are treated with routine antibiotics, at least in the United States, and the illness almost seems extinct. The annual incidence of tuberculosis decreased to 2.8 cases per 100,000 people in 2018, with little over 9,000 new cases reported, as per the most recent data available from the Centers for Disease Control and Prevention.
“It’s easy to view TB as a forgotten disease in the U.S., but it was not that long ago that TB was a primary cause of disease here,” says Dr. Lisa Chen, principal investigator and medical director of the Curry International Tuberculosis Center at the University of California, San Francisco. “Almost every family has a story to tell if you ask grandparents or great-grandparents.” Globally, by contrast, TB remains an ongoing scourge. In 2018, a total of 1.5 million people died from TB, according to the World Health Organization. An estimated 10 million people fell ill with TB worldwide, including 1.1 million children.
Types of tuberculosis
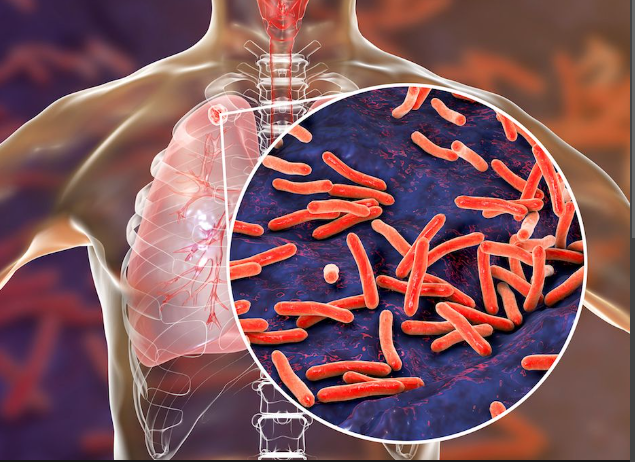
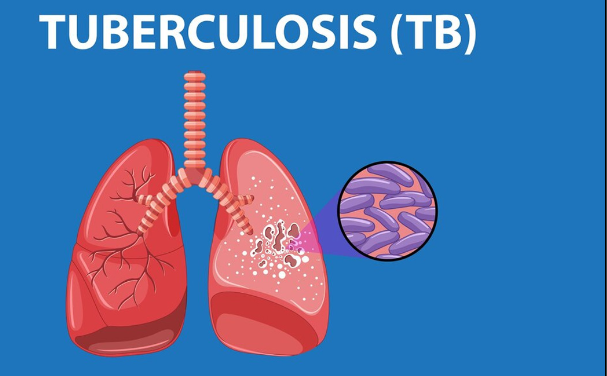
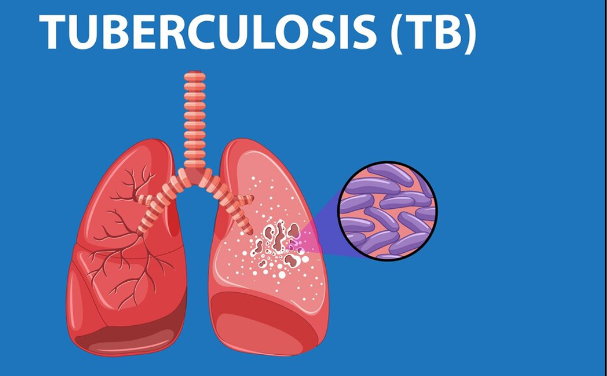
Many more people are infected with Mycobacterium tuberculosis, the bacteria that causes TB, than people who actually become sick and exhibit symptoms of the respiratory disease.
Latent tuberculosis Infection
When people are infected with M. tuberculosis but don’t feel sick or have any symptoms, it’s called a latent TB infection. Although they do have TB bacteria in their bodies, these bacteria are inactive. People with latent TB are not contagious; they cannot spread the bacteria to others around them. Many people who have a latent TB infection are unaware of it. “There are an estimated 13 million people infected with TB in the U.S., and 1 in 10 of those individuals is likely to go on to develop TB disease,” Chen says. People in occupations that pose a higher risk for TB exposure and transmission, like health care workers in hospitals, may undergo routine screening. Others who are known to be in close contact with someone who’s been diagnosed with infectious TB, such as family members or friends, may be screened as well.
Active TB Disease
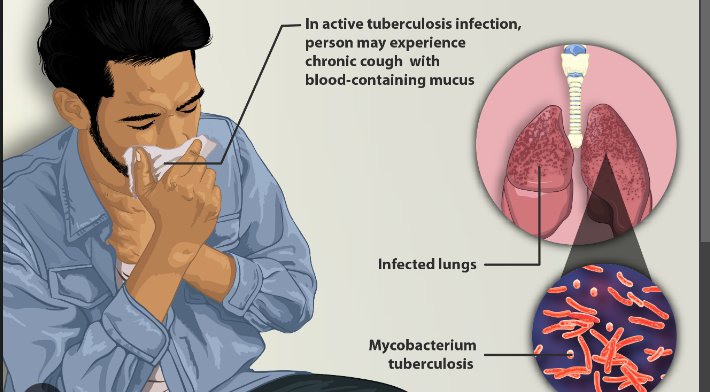
With active tuberculosis , people are infected with TB bacteria and they feel sick. They’re experiencing symptoms such as unexplained weight loss, night sweats, fever and chills, and a persistent cough. People with active disease can spread TB bacteria to others. Untreated TB can be fatal. If screening or routine testing reveals that you have a latent TB infection, preventive treatment is recommended. Without antibiotic treatment, between 5% and 10% of people with latent TB eventually develop active TB disease. The risk is higher for people with weakened immune systems, such as those with HIV infection.
Causes
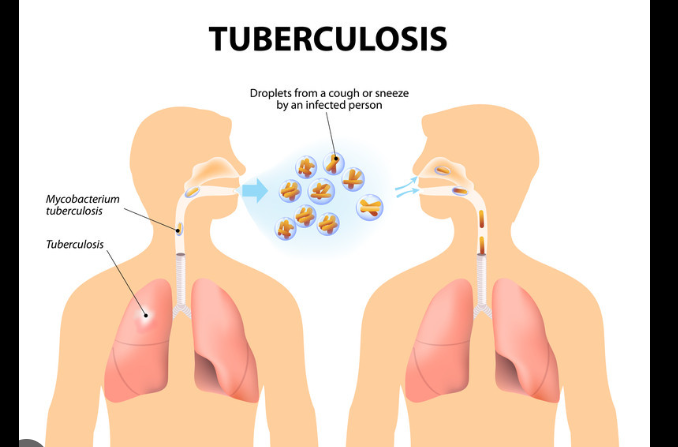
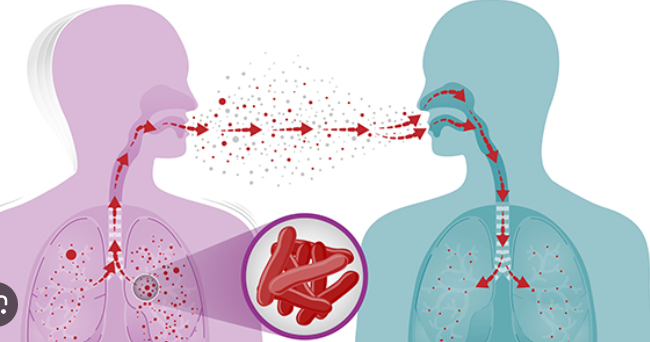
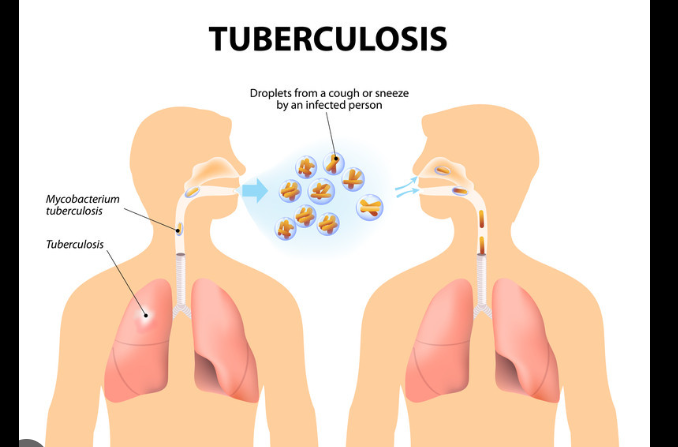
Tuberculosis germs spread when somebody who has active TB disease coughs, sneezes, or laughs, and a nearby person breathes in those droplets. “Because TB is spread through the air, the risk is highest for those who spend a lot of time in the same confined place,” Chen says. The risk is lower where there’s good ventilation with more open space versus poorly circulated air that people continually share and breathe. Casual exposure on a bus, subway, or even a plane is not likely,” Lardizabal says. Similarly, you’re unlikely to get infected at the grocery store or mall. “The more prolonged the contact is, and the more that air is not exchanged—essentially using the same stale or recirculated air—that increases the transmission,” he says.
Risk factors
People who have compromised immune systems are more vulnerable to developing active disease and getting infected with tuberculosis. HIV infection, diabetes, kidney failure, substance abuse, and normal aging all have a tendency to compromise immune function. The increasing number of people using medications that alter the immune system is another factor to consider, according to Chen. Patients undergoing transplants and those receiving some of the more recent treatments for autoimmune diseases fall into this category.
Symptoms
Persistent coughing is the most common symptom of TB. “It may start off like a cold with a cough, but then it does not go away,” Chen says.
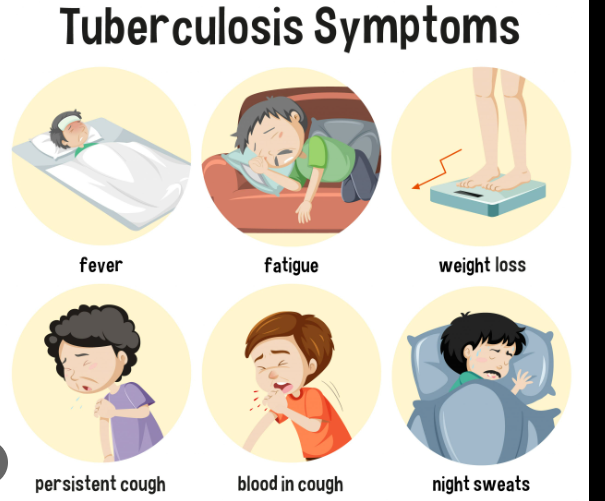
For active tuberculosis disease, these are the classic symptoms:
- Cough that lasts more than a week or two.
- Coughing up blood.
- Unexplained weight loss.
- Fatigue.
- Night sweats from low-grade fever.
Because many TB symptoms are nonspecific—there could be a variety of causes—it makes it difficult for people to get diagnosed in a timely fashion, Flynn says. As symptoms like weight loss develop quite gradually, the sense of urgency to see a doctor might not be there. With advanced TB, symptoms are more obvious, making it clear why the disease was once commonly called consumption. “When I’ve visited TB hospitals around the world, when you see someone who has TB, it does appear that they’re being consumed by something,” Flynn says. “They get a gaunt look; they might be flushed.” In old movies, coughing up blood was a giveaway that a character was stricken with TB. It’s still a tell-tale symptom. “I always tell my medical students: If you see somebody who’s coughing up blood, they probably have TB,” Flynn says.
Diagnosis
Screening people at higher risk of tuberculosis infection is often the first step toward diagnosis.
According to the CDC, certain people are considered for testing due to their higher risk, such as:
- People who have had close contact with someone who has TB disease.
- People who live or work in high-risk settings, including long-term care facilities or nursing homes, homeless shelters, and correctional facilities,.
- Health care workers who take care of patients are at higher risk for TB disease.
- People born in, residing in, or traveling from a country where TB is common. That includes almost every country except for the U.S., Canada, Australia, New Zealand, and countries in Northern or Western Europe.
- Infants, children, and teens who are exposed to adults are at increased risk of TB disease or latent TB infection.
- People with suppressed immune systems, such as those with HIV, organ transplant recipients, those on chronic steroid treatment or those being treated with certain immune system-modifying drugs,.
Tests
Skin Test
A standard tuberculosis skin test involves a shallow injection of a small amount of fluid, called a tuberculin-purified protein derivative, just beneath the skin surface of the forearm. This subcutaneous injection, or PPD test, is also called a Mantoux tuberculin skin test. Within two to three days, you must make a return visit so your health care provider can check the injection site on your arm for a reaction. The site will be examined for a raised, hardened, or swollen area, called an induration, which is measured. An induration of 15 or more millimeters is considered positive for someone who has no known risk factors for TB. If you have a positive skin test, it’s not a cause for alarm. “It only tells you whether you’ve ever been infected,” Flynn points out. “It doesn’t tell you whether or not you have active TB or latent TB.”
Blood Test
Blood tests are sometimes used to detect TB. For instance, people who have received the BCG vaccine for TB (which is not used in the U.S.) should have a blood test instead of a skin test. Blood testing may be more practical for people who have a difficult time returning for the second appointment to check their skin reaction. TB blood tests are also known as interferon-gamma release assays. With a positive TB test, you move on to the next diagnostic criteria. Diagnostic tests could include:
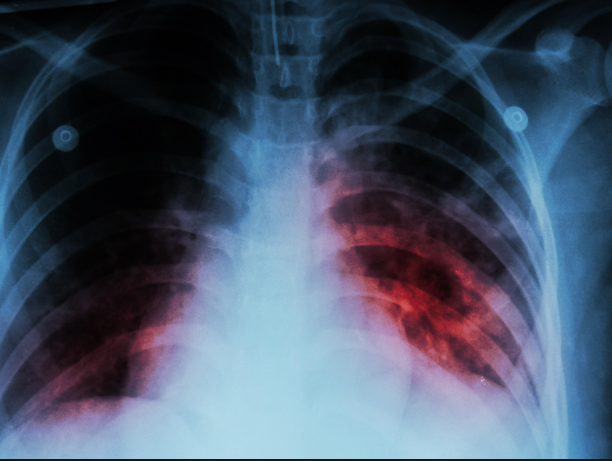
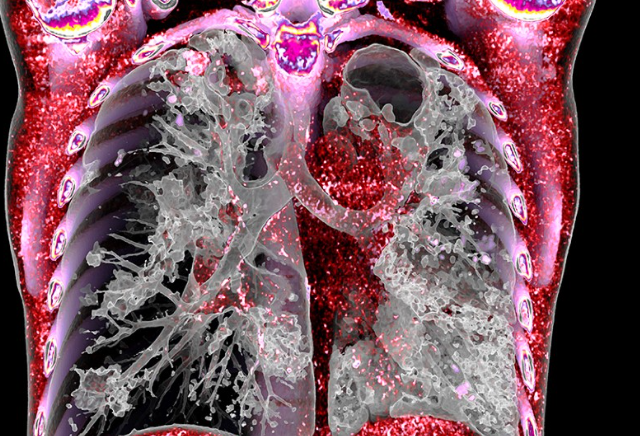
- Chest X-ray or chest CT (less frequently) to reveal any lung changes.
- Sputum culture: “Sputum is basically coughing stuff out of your lungs, Flynn says. “Then we would culture that for Mycobacterium tuberculosis.”
It can take two weeks or more before sputum culture results are available. If a sputum culture is positive, treatment planning begins.
Treatment
Antibiotics are the primary treatment for both latent TB infection and active TB disease. However, the number of antibiotics used and specific timetables are different. These are the four antibiotics used to treat TB:
- Isoniazid.
- Rifampin.
- Pyrazinamide.
- Ethambutol.
Also read-Unveiling The Marvels Of Biotin: A Comprehensive Guide To Radiant Hair And Nails
images source: Google
Disclaimer: The opinions and suggestions expressed in this article are solely those of the individual analysts. These are not the opinions of HNN. For more, please consult with your doctor