Weight-loss bariatric surgery can have profound effects on your health, appearance and lifestyle.
Weight-loss methods that are optional are included in bariatric surgery. In certain situations, it can even treat obesity-related illnesses like type 2 diabetes. It can have dramatic effects, enabling severely obese people to drop significant excess weight.
Surgery for weight loss isn’t appropriate for everyone, though. In order to qualify for surgery, you have to fulfill a few requirements. Additionally, bariatric surgery requires dedication and is by no means simple. To sustain your weight loss and health improvements, you must make long-term dietary and drinking adjustments.
Also read-6 Myths Around Childhood Cancer You Need To Know

How to qualify
Patients must generally meet certain criteria to undergo bariatric surgery. You could be a candidate if you fall under one of these categories, as outlined by ASMBS:
- You are either at least 100 pounds overweight or your body mass index (BMI) is at least 40.
- You have at least one obesity-related medical condition and a BMI of at least 35.
- In past attempts at weight loss, you have not been able to reach or maintain a healthy weight loss.
Weight-loss surgery may be beneficial for illnesses connected to obesity, such as sleep apnea, osteoarthritis, heart disease, gastrointestinal issues, Type 2 diabetes, and hypertension. Using this online calculator from the Centers for Disease Control and Prevention, you can determine your BMI.

Types of bariatric surgery
When it comes to weight-loss surgery, less is more. With reduced stomach volume, you eat less food and lose more weight. Each type of bariatric surgery takes a different approach. These are the most commonly used procedures:
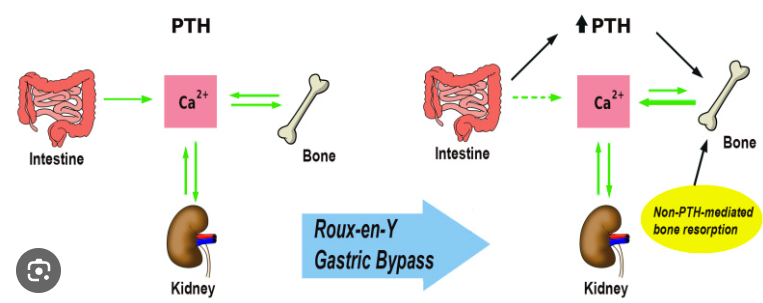
- Gastric bypass. Roux-en-Y gastric bypass, often simply called gastric bypass, reduces the size of your stomach. Surgeons create a small pouch using the top part of your stomach. This reduces the amount of food you can consume. Bypass involves connecting a small portion of your small intestine, or jejunum, to a hole in your pouch. That way, food can travel directly from the pouch into your small intestine, allowing you to absorb fewer calories.
- Sleeve gastrectomy. In a vertical sleeve gastrectomy, about three-quarters of your stomach is surgically removed. What remains is a tube- or sleeve-shaped section, which can only contain a fraction of the food it used to.
- Duodenal switch. With a duodenal switch, your stomach absorbs less food. Officially known as biliopancreatic diversion with duodenal switch, this approach combines some features of sleeve gastrectomy and bypass. It’s usually done as an open procedure. In some cases, the duodenal switch is performed in two stages, several months apart. As a more complex procedure with potentially more risk involved, it’s less frequently used than gastric bypass or sleeve gastrectomy, De Maria explains. “Also, the long-term management can be challenging because these patients have so much weight loss that they can actually have malnutrition.”
- The lap band. An expandable balloon is inserted around the top of your stomach as part of a laparoscopic gastric banding procedure, also known as an adjustable gastric band. This effectively divides your stomach into two pieces. You are limited to eating what will fit inside the top section. But gradually, the food enters the lower part of the stomach through the band, enabling regular digestion.
Risks and side effects
Because most bariatric surgeries are now done as minimally invasive, laparoscopic procedures, major risks have decreased from when they were largely performed as traditional surgery, De Maria says. These are some short-term surgical side effects or complications you could experience:
- Nausea and vomiting after general anesthesia.
- Surgical incisions cause soreness or pain.
- Infection.
- Bleeding.
- Gastrointestinal leakage.
- Blood clots.
- Dumping syndrome.
- Dehydration.
- Malnutrition.
- Ulcers.

Benefits
Bariatric surgery can benefit patients on multiple levels, both as therapy and as prevention. “Individuals who undergo bariatric surgery are doing so in an effort to lose weight, so it’s therapeutic to help them do so,” says Dr. John Daly, co-chair of the patient education committee for the American College of Surgeons and a surgical oncologist at Fox Chase Cancer Center in Philadelphia.

Bariatric procedures can also be preventative for people with prolonged obesity, who are at increased risk of having high blood cholesterol and higher rates of atherosclerosis, stroke and heart attacks, Daly says. With weight-loss surgery, those risks are reduced. “If they have diabetes, most oftentimes the diabetes is reversed—they no longer have diabetes.

Where to have surgery
Selecting a specialized, high-volume clinic that specializes in bariatric medicine and surgical treatments makes sense, just like with other types of surgery. De Maria advises people to look for a recognized facility to have bariatric surgery. “Accredited centers are evaluated every three years, and their outcomes are looked at and scrutinized, so we know they meet the standards,” according to him.

Also read-In the New Year, California Will Increase Low-Income Immigrants’ Access To Health Care
images source: Google
Disclaimer: The opinions and suggestions expressed in this article are solely those of the individual analysts. These are not the opinions of HNN. For more, please consult with your doctor




































