The incidence of endometrial cancer is rising. However, life is saved by early detection.
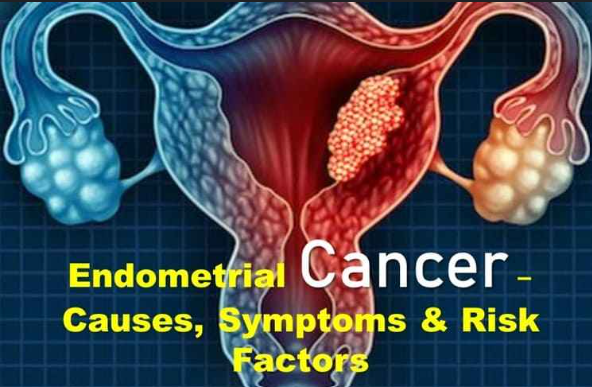
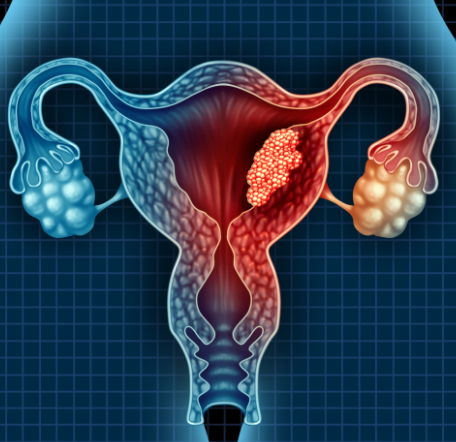
The incidence of endometrial cancer, which arises in the uterine lining, is increasing.
According to the most recent trending data from the Centers for Disease Control and Prevention, uterine cancer incidence rates rose by 12% between 1999 and 2015, partly due to the obesity pandemic. This rise distinguishes endometrial cancer, the most prevalent type of uterine cancer, from numerous other malignancies that are becoming less prevalent.
According to the American Cancer Society, over 12,000 women will lose their lives to uterine cancer this year, and over 62,000 new cases will be identified. According to the American Cancer Society, it is also the most prevalent cancer that affects female reproductive organs.
Being overweight increases a woman’s risk of endometrial cancer by causing her to produce more estrogen. According to Dr. Mehdi Kebria, a gynecologic oncologist at City of Hope, a comprehensive cancer center located in Duarte, California, close to Los Angeles, the ovaries produce the hormones estrogen and progesterone, which have an impact on the endometrium. “The endometrium thickens as a result of excessive estrogen exposure, and endometrial cancer may eventually result from prolonged exposure to high levels of estrogen.”
Causes
The risk of endometrial cancer is increased by being overweight and related diseases like Type 2 diabetes and high blood pressure. Among the risk factors for this malignancy are:
- Being overweight.
- Diabetes.
- Age: As you age, your risk increases.
- Having close family members with colorectal or endometrial cancer, such as a parent or sibling.
- Exposure to the hormone treatment medication tamoxifen, which is used to treat breast cancer.
- Lynch syndrome is a hereditary disease.
A woman with Lynch syndrome has a significantly higher chance of getting endometrial cancer in addition to an increased risk of other cancers like ovarian and colon cancer. It is advised that people who have a first-degree relative with Lynch syndrome—such as a parent, sibling, or child—get genetic testing to see if they are more likely to develop endometrial cancer and other cancers.
Prevention
To avoid uterine cancer, some women with Lynch syndrome choose to have their uterus surgically removed—a procedure known as a hysterectomy. However, experts emphasize that choices about prevention and treatment should be chosen individually and guided by consultation between the woman and a physician who specializes in treating uterine cancer, such as a gynecologic oncologist.
To lower the risk of cancer, it is recommended that everyone maintain a healthy weight. Research indicates that weight loss is linked to a decreased risk of endometrial cancer, especially for obese postmenopausal women.
“In overweight women, weight loss and a well-balanced diet can lower the risk of endometrial cancer,” says Kebria. He adds that using progesterone-releasing intrauterine devices (IUDs), another type of birth control, and oral contraceptives can help lower the risk of endometrial cancer.
Symptoms Of Endometrial Cancer
Early detection of this cancer greatly improves the prognosis for patients and can ultimately help them outlive it. The American Cancer Society estimates there are more than 600,000 endometrial cancer survivors in the U.S. today.
Possible signs of this cancer to look for are:
- Unusual vaginal bleeding or spotting.
- Abnormal vaginal discharge, even without bleeding.
- Pelvic pain.
- Painful urination.
- Unexplained weight loss
Diagnosis
If you experience unusual vaginal spotting or bleeding, seeing your gynecologist for an evaluation that includes a pelvic exam is a good place to start.
Depending upon your symptoms or if you’re at higher risk for endometrial cancer, a variety of different tests may be done to determine if you could have endometrial cancer. That could include:
- Endometrial biopsy.
- Transvaginal ultrasound.
- Hysteroscopy.
- Imaging like a CT scan for cancer that may have spread.
Treatments
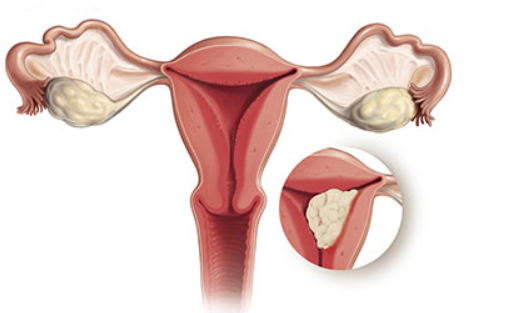
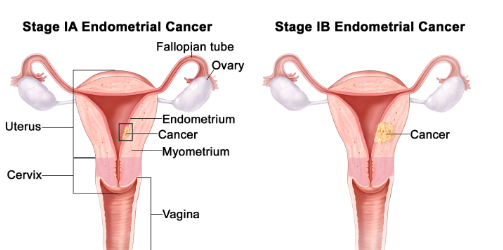
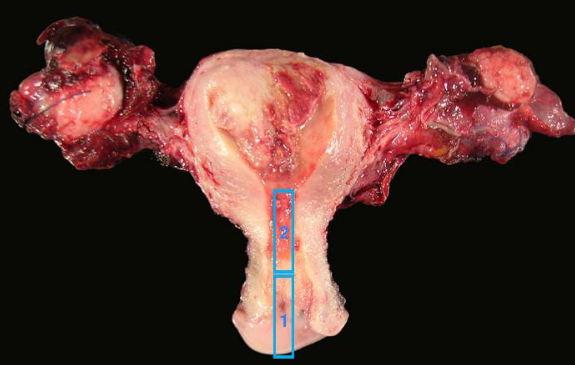
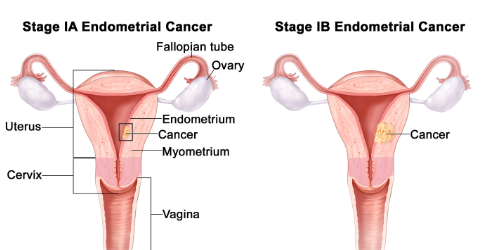
To best gauge a patient’s prognosis and options for treating endometrial cancer, staging is critical.
Stage 1 endometrial cancer, for example, is limited to the uterus and perhaps glands of the cervix. The most advanced form, stage 4 endometrial cancer, has spread well beyond the uterus and could be in “distant sites,” ranging from the lungs to the liver to the bones.
Fortunately, endometrial cancer is usually caught in stage 1. And the treatment for this uterine cancer is commonly surgery to remove the uterus. The modern procedure tends to be minimally invasive, done through small incision sites to lessen pain afterward and speed recovery.
Depending upon the extent of the cancer, the ovaries and, in some cases, the surrounding lymph nodes (immune system glands) are removed as well. “In some cases, if the cancer is found to have spread beyond the uterus, use of chemotherapy or radiation therapy after hysterectomy may become necessary,” Kebria says.
For some premenopausal women with endometrial cancer who want to maintain the ability to have children, hormonal therapy may be an option. “Hormonal therapy can be effective in managing a selected group of young patients with less aggressive and early stage endometrial cancer who are interested in fertility preservation,” Kebria says.
With this approach, patients take progesterone orally for six to nine months, he says, and their response to the treatment is assessed using ongoing imaging and biopsies. “Unfortunately, this approach is not always successful, and in some cases, a hysterectomy is inevitable,” Kebria notes.
For most women who have stage 1 endometrial cancer that’s successfully treated, the cancer doesn’t come back. “The majority of those patients will do just fine and be cured of their cancer,” Matulonis says.
Also read: Women’s Asian Champions Trophy 2024 hockey
images source: Google
Disclaimer: The opinions and suggestions expressed in this article are solely those of the individual analysts. These are not the opinions of HNN. For more, please consult with your doctor