Engaging in any form of physical activity can help avoid blood clot because it maintains blood flow. Learn techniques to make getting back into the gym easier.
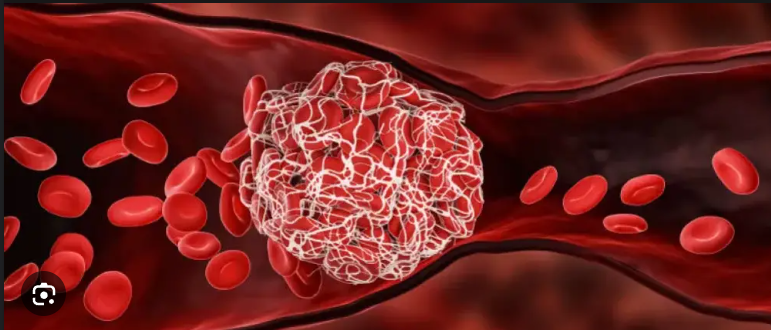
If you’ve ever scraped your knee from falling, you know that blood clots eventually stop the bleeding. Nature uses clotting to help stop the blood flow from a cut or wound.
Also read-Ulcer Diet: What To Eat And What To Avoid For Healthy Life
More precisely, bleeding results from damage to small blood vessels following a superficial cut. In response, the body activates platelets, which are microscopic cells that clog blood vessels. A scab forms over the wound, indicating that the clotting process has ended in your body. However, blood can clot inside the body, which can be harmful.
What is a blood clot?
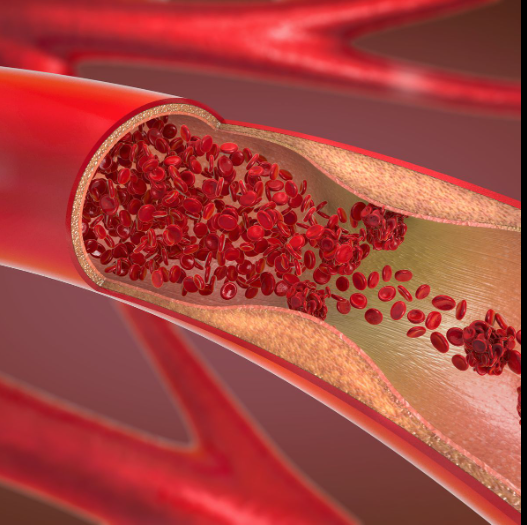
Internal blood clots are collectively referred to by medical professionals as “venous thromboembolism,” or VTE. A VTE typically happens in one of two ways:

- Deep vein thrombosis, or DVT, is a clot that forms in a deep vein, most often in the leg. Often, signs and symptoms include redness, warmth, or tenderness in the affected area. The pain typically worsens with movement and feels like a cramping sensation.
- Pulmonary embolism, or PE, is a complication of a DVT. A PE occurs when a clot breaks free and lodges itself into a vessel that supplies the lungs. This clot then blocks the lung’s blood flow. A PE usually manifests as sudden shortness of breath or chest pain.
VTEs are common; the CDC estimates more than 900,000 people are affected by them each year. They’re often diagnosed with a combination of symptom evaluation, imaging results, and a blood test.
Risk factors for blood clots
Blood clots can be fatal, so it’s important to understand what puts you at risk. The Society for Vascular Medicine groups potential causes and risk factors for VTEs into five main categories:
- Immobility. Hospitalization and long-distance travel that requires sitting for more than eight hours are common culprits. This is why movement and exercise can help prevent blood clots (more on that later on).
- Incisions or injuries DVTs and orthopedic surgery are frequently linked, particularly in the case of large joint replacements. The body must clot in order to heal itself after traumatizing itself, such as breaking a bone or rupturing a muscle. The body can overreact to clotting occasionally, which can result in VTEs.
- Elevated estrogen. The risk of VTE can be raised by hormonal birth control, during pregnancy and the postpartum period, and by hormone replacement therapy.
- Health issues. Cancer and inflammatory conditions like lupus and irritable bowel syndrome may fall into this category.
- Genetics and lifestyle VTE risk is elevated in families with a history of clotting disorders or blood clots. Additionally, significant risk factors include lifestyle choices like smoking, being obese, leading a sedentary lifestyle, or being 60 years of age or older.

For patients who already have DVT, all of the above risk factors also put them at risk of dislodging their clot to become a potentially life-threatening pulmonary embolism. However, DVT and VTE can be caught early and are often treated successfully with anticoagulant “blood-thinner” medication like warfarin or with surgery.
Exercise after a blood clot
Once your DVT or VTE is treated, you should maintain or begin a more active lifestyle.
“You want people to exercise because the lack of exercise causes clots,” explains Ellen Hillegass, a physical therapist with American Physical Therapy Association board certification in cardiovascular and pulmonary clinical specialty. She also serves as a professor in the physical therapy department at South College in Atlanta.
However, you should ease into an exercise program, says Dr. Geoffrey Barnes, a cardiologist and president-elect of the Anticoagulation Forum. Barnes is also a vascular medicine specialist at the University of Michigan.
Barnes recommends avoiding vigorous exercise in the first week after a DVT and two weeks after a PE. Following these more restful periods, patients can slowly and steadily ramp up their activity levels.
After that? “Any exercise,” Hillegass recommends.
If you want to work the entire circulatory system, you might consider aerobic activities, such as:
- Walking.
- Running.
- Biking.
- Swimming.
Sample Workout Plan After a Blood Clot
As long as your doctor gives the all-clear, walking is a great way to resume your exercise regimen, according to the North American Thrombosis Forum, or NATF. Generally speaking, you want to choose a walking route that is reasonably level, close to your house, and has rest stops along the way, like a park.

Warm up with a slow walk for five minutes, then increase your activity each week.
- Week 1: Walk for five minutes at a comfortable pace, three to four times per day.
- Week 2: Walk for 10 minutes, three times per day.
- Week 3: Walk for 15 minutes two times per day.
- Week 4: Walk for 30 minutes, once daily.
Set a goal to walk for 30 to 45 minutes, five to seven days per week.
Strength training is important for maintaining physical health as well, according to NATF, and if you already practice strength training, you can safely resume your regular schedule. Ask your primary care physician for a recommendation to a licensed physical therapist or trainer if you don’t already have one and would like to start. They can collaborate with you to design a customized strength training program.
Moving forward after a blood clot
There are multiple strategies you can try to make exercising after a blood clot more pleasant.
Hillegass recommends approaches like:
- Reducing pain and swelling by donning compression stockings.
- Commencing with exercises that do not require lifting weights, like riding or swimming,
- See what feels comfortable by experimenting with different types of exercise.
As you’re exercising, though, you should be on the lookout for shortness of breath.
“If you had a pulmonary embolism, you can get a condition called chronic thromboembolic pulmonary hypertension,” Hillegass warns.
CTEPH is a rare and progressive form of pulmonary high blood pressure caused by blood clots that don’t dissolve in the lungs, according to the CHEST Foundation. These clots cause scar-like tissue that clogs up or narrows the small blood vessels in the lungs.
“If you develop shortness of breath, you should be evaluated by a pulmonologist,” Hillegass says.
Your provider should also provide close medical follow-up after a blood clot to ensure your health is improving, Barnes adds.
“Your doctor will review your medications and how well you are recovering,” he explains. “Staying active, including regular exercise, is a great way to reduce your risk of future blood clots by helping to keep the blood in your legs circulating properly.”
Also read-Ulcer Diet: What To Eat And What To Avoid For Healthy Life
Disclaimer: The opinions and suggestions expressed in this article are solely those of the individual analysts. These are not the opinions of HNN. For more, please consult with your doctor.
images source-google




































