Bursitis, a common injury, can often be alleviated with rest and physical therapy
The human body has numerous intelligent defense mechanisms to keep itself safe. The body is capable of self-defense, from the skin, which serves as a general barrier against external threats, to the immune system within, which tracks down and eliminates foreign infectious agents that manage to get through openings in the skin.
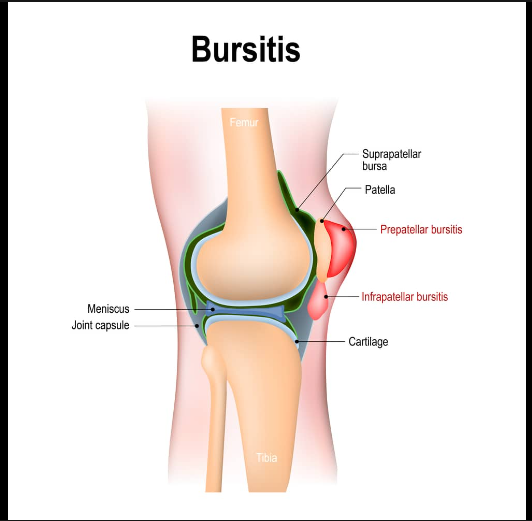
Bursa offers a portion of those defense components. “A bursa is a layer of tissue that covers a tendon or bone and helps the tissue below glide or be protected in its motion,” explains Dr. Taylor R. Dunphy, a sports medicine specialist and orthopedic surgeon at the Hoag Orthopedic Institute in Newport Beach, CA. The bursa protects joints and other body parts that allow for normal motion, and “it’s kind of like a gliding structure that aids in tendon motion.”
Also read-Parkinson’s Disease : A Patient’s Guide To Parkinson’s Disease And Its Symptoms
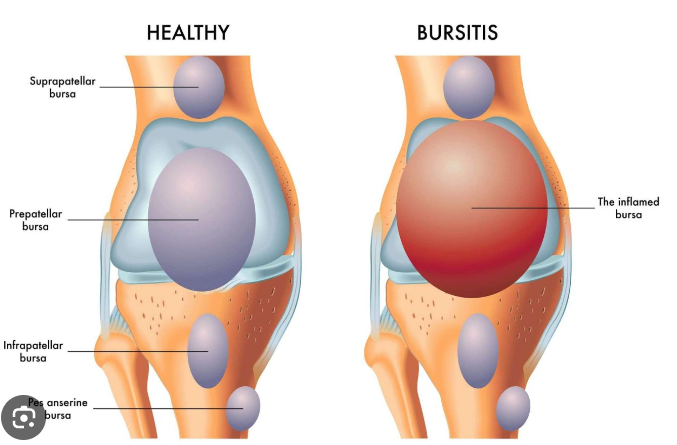
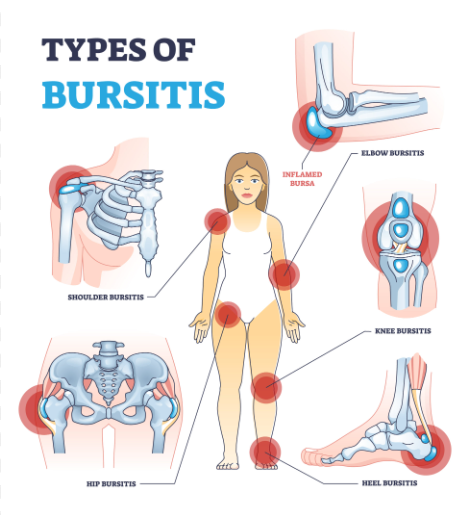
The bursa is “a fluid-gel padding sac that allows some of the soft tissue to slide over the top of a more prominent boney area more smoothly,” according to Dr. W. Kelton Vasileff, an orthopedic surgeon and sports medicine specialist at The Ohio State University Wexner Medical Center. The body contains over 150 bursa, the most noticeable of which are found in the main joints: the shoulders, elbows, hips, and knees.
The bursas are intended to shield vital joints and tendons from harm, but under some circumstances, they can become problematic and result in bursitis.
What Is Bursitis?
Anytime you add the suffix “itis” to a body part, it means there’s inflammation in that area, so bursitis is simply inflammation of the bursa. It can occur in any of the bursa throughout the body, but more commonly occurs in the large joints, Dunphy says, including:
- The shoulder. Subacromial bursitis often occurs because of an impingement, like a bone spur, or because of damage to the rotator cuff, an important group of tendons that control movement in the shoulder, especially when performing overhead activities.
- The elbow. Olecranon bursitis typically results from a trauma, such as falling and landing hard on the bony point of the elbow, or from placing repetitive pressure on the bursa, as may occur when leaning on your elbows a lot.
- The hip. Trochanteric bursitis occurs in the outer part of the hip joint and is common among runners who place a lot of repetitive strain on the joint and may have a tight iliotibial band (a thick rope of tissue that runs from the outside of the hip to the knee and stabilizes knee and hip movement) that places further stress on the area. Bursitis in the hip may also be associated with a condition called greater trochanteric pain syndrome, or gluteal tendinopathy.
- The knee. Prepatellar bursitis occurs in the bursa that lies over top of the patella or kneecap. There are several other bursas in the knee, but the prepatellar bursa is the one where bursitis is most likely to develop and often crops up in athletes who have fallen on the knee or in people who kneel a lot as part of their job, such as carpenters or gardeners.
“There’s a lot of different reasons that you could have bursitis,” Vasileff says. “It could be from some kind of injury, which would be called traumatic bursitis. Or it can result from an overuse issue. Or it could be just an inflammatory issue as well.”
Risk factors
Bursitis is often related to trauma or overuse; it’s a common injury among certain kinds of athletes. “There are different origins for bursitis,” Dunphy says. “For the knee or the elbow, it’s usually a trauma. With the shoulder and hip, it’s usually a repetitive motion, so in those cases, someone who does repetitive stuff is more likely to develop it,” he says.
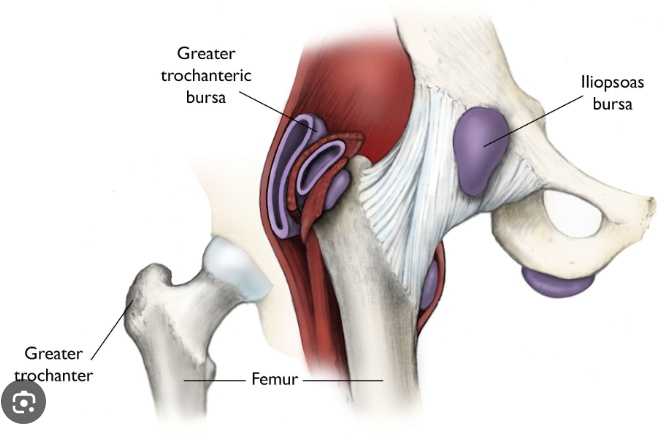
For example, “if you’re a wrestler or football player going down on the knees, you may develop prepateller bursitis. For the hip, that would be more runners. As you run, that tissue rubs over the edge of the top of the femur, and that irritates the bursa. A classic scenario is runners who train indoors on a banked track—that banked surface irritates the IT band,” adding tightness and pressure in the hip area that can lead to bursitis.
Lastly, with shoulder bursitis, “people who do overhead activities,” such as swimmers or throwers, are more likely to develop that problem, particularly over time. “As you get older, you start to get bone spurs under the acromion (a bony part of the shoulder that sits at the end of the clavicle and above the humerus arm bone), and when you’re doing arms-up, overhead work, that can irritate the bursa or the rotator cuff,” Dunphy says. Carpenters and painters who have to reach overhead a lot may develop bursitis in the shoulder.
Diagnosis
Vasileff says bursitis is sometimes an obvious diagnosis to make and is based on a clinical exam. One of the most telling symptoms is when a patient complains of a specific type of pain in specific locations or notes that certain activities provoke it. “The distinctness of the pain, the character of the pain tends to be a little different” from some other conditions, and when “somebody comes in complaining of pain in a certain area of the elbow, that’s pretty distinct. A lot of times when I see patients with hip problems, they’ll complain of much more pain on the side of the hip because that’s where the main bursa area is as opposed to the hip joint itself.” He says if the pain is felt deeper inside the joint or on the front of the hip, that’s likely caused by something other than an inflamed bursa.
Treatment
Most cases of bursitis can be treated with simple interventions, Dunphy says, and it’s best to start with a conservative approach. “Anti-inflammatories like ibuprofen (Advil, Motrin) and using an Ace wrap to provide compression can help the fluid reabsorb,” he says. Immobilizing the area to prevent further irritation can also help, so for patients with bursitis in the elbow, a splint might be a good option to give it the time it needs to heal.

If a case of bursitis has resulted from a trauma rather than an underlying impingement, rest and time are often the best treatments. For example, if a soccer player falls hard on her knee and develops swelling and pain on top of the kneecap without any other injury to the tendons or bones, “in those situations, the approach is usually rest, compression, ice, anti-inflammatories, and things like that. Rarely will we drain those,” Vasileff says, because the fluid that results from the inflammation can easily build back up.
Also read-Diet And Arthritis: What To Avoid In Foods For Good Health And Happy Life
images source: Google
Disclaimer: The opinions and suggestions expressed in this article are solely those of the individual analysts. These are not the opinions of HNN. For more, please consult with your doctor.