Know the basics of symptoms, diagnosis, and treatment to help in cardiomyopathy with heart muscle disease.
Cardiomyopathy is a dangerous illness characterized by the weakening of the heart muscle. Cardiomyopathy can be caused by a variety of conditions that directly impact the structure, pumping capacity, and function of the heart muscle.
There are numerous ways that it manifests. It usually occurs after coronary artery disease or a heart attack, frequently in middle-aged men. Rarely does it manifest itself on football fields or basketball courts, where young athletes who suffer from undetected pain die.
Also read-Macular Degeneration : A Patient’s Guide To Macular Degeneration And Its Symptoms
During pregnancy, a woman’s symptoms can masquerade as normal effects of gestation. Broken heart syndrome, or takotsubo cardiomyopathy, sometimes results from severe physical or emotional stress. Cardiomyopathy can be temporary with complete recovery but more typically becomes a chronic condition.
Symptoms of cardiomyopathy
There may be no warning signs in the early stages. As it gradually worsens, you may have the following signs and symptoms:
- Shortness of breath with exertion.
- Swollen feet, ankles, and legs.
- Tiredness and fatigue.
- Difficulty lying flat: needing to prop your head on pillows or waking up gasping for air.
- Dizziness and lightheadedness.
- Heart palpitations.
- Chest pain.
- Fainting or syncope.
- High blood pressure.
Types and causes
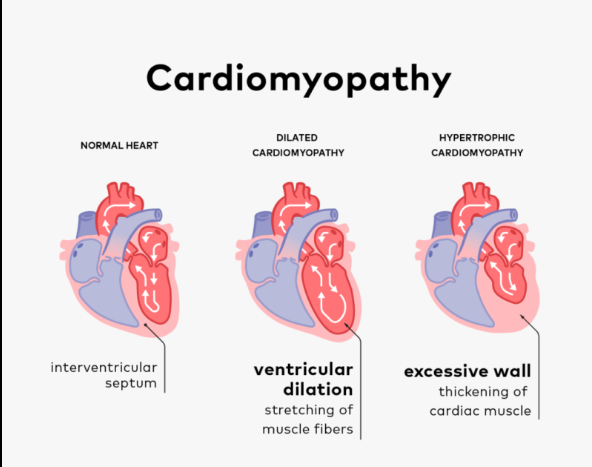
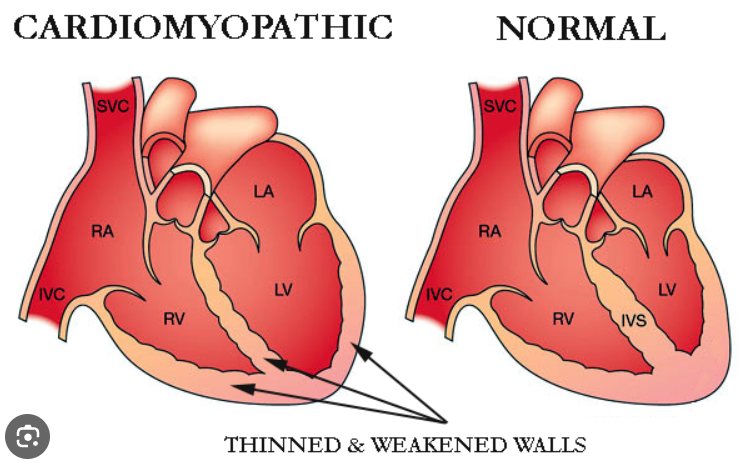
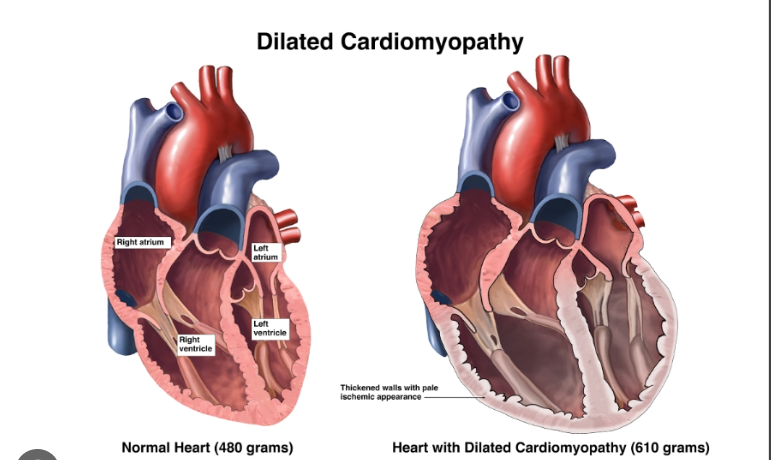
Cardiomyopathy dilated. The American Heart Association states that adults between the ages of 20 and 60 are most likely to experience this. Among the leading causes are diabetes, high blood pressure, heart disease, and heart attacks. There are instances where the illness runs in families. There are no known causes in other cases.
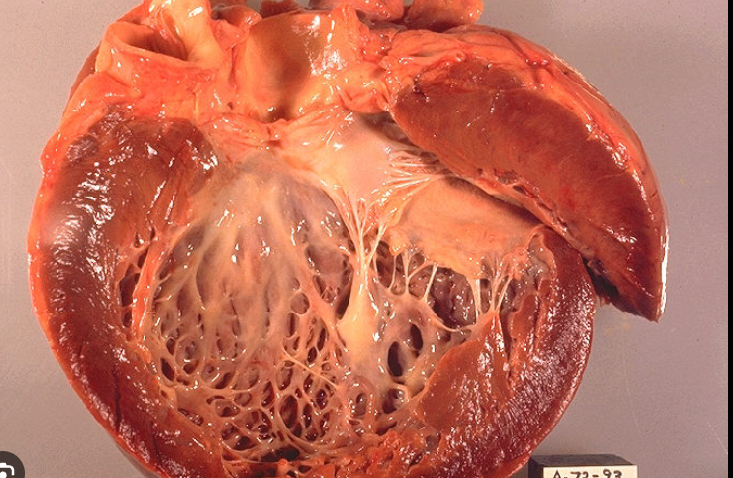
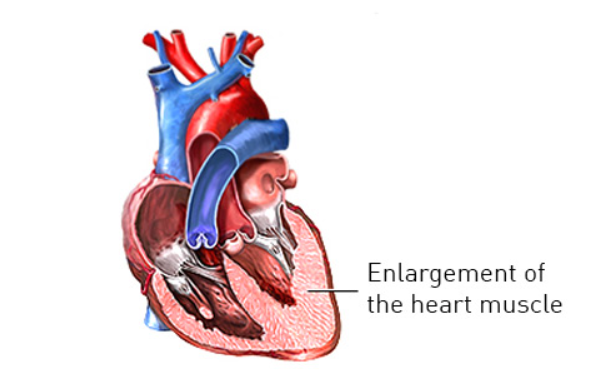
The lower left ventricle, the main pumping chamber, becomes stretched, thin, and eventually enlarged in dilated it, weakening the heart. The heart’s capacity to pump correctly is lost as the issue deepens. Possible complications include abnormal heart rhythms, arrhythmias, heart failure, and blood clot formation.
Hypertrophic heart disease. People of any age can be affected by this condition, which usually runs in families. According to the AHA, hypertrophic cardiomyopathy affects up to 500,000 people in the United States. Hypertrophic cardiomyopathy is characterized by abnormally thick ventricle walls and a possible blockage of outward blood flow to the aorta. Rarely, the illness may cause dangerous arrhythmias when engaging in very strenuous physical activity. A mid-2016 overview study found that the most common cause of sudden cardiac arrest in athletes is hypertrophic cardiomyopathy.
Broken-heart syndrome, or Takotsubo cardiomyopathy. The illness, which was initially discovered in 1990, is typically brought on by extreme stress, which weakens the left ventricle of the heart. It’s been connected to stressful events that cause abrupt increases in stress hormones, like the death of a loved one or even seemingly good things like surprise parties. After menopause, older women are more vulnerable to takotsubo cardiomyopathy due to hormone drops like estrogen. Takotsubo can occasionally be lethal.
Takotsubo cardiomyopathy is, fortunately, typically transient and nonfatal. Dr. Pamela Douglas, a professor of research in cardiovascular diseases at Duke University in Durham, North Carolina, says, “Most of the time it gets better.”
Peripartum cardiomyopathy. This develops during pregnancy or soon after. “It’s a type of cardiomyopathy where the connection is pregnancy and we don’t think there’s some other cause,” says Dr. Melinda Davis, a cardiologist at Michigan Medicine’s Frankel Cardiovascular Center.
The condition can be confusing because symptoms of heart failure are often similar to those of normal pregnancy, says Davis, who is also an assistant professor at the University of Michigan. “Normally, during pregnancy, women develop swelling and shortness of breath and it’s very common,” she says. “That’s why peripartum cardiomyopathy can be difficult to diagnose and women sometimes don’t get diagnosed right away.” If the possibility of cardiomyopathy exists, she adds, a simple blood test called a BNP, which measures levels of a protein produced in the heart, can help screen women who need further evaluation.
Diagnosis of
A physical examination and a thorough medical and family history are the first steps in the diagnosis of cardiomyopathy. Your physician will ask about symptoms and when they occur, such as while you’re lying down or when you’re exercising. Because cardiomyopathy can have a strong genetic connection, you may be asked about heart disease among your close relatives.
Tests you undergo would likely include a chest X-ray to detect heart enlargement, an echocardiogram to show images of your heart with ultrasound, and an electrocardiogram, or EKG, to look for problems like abnormal heart rhythms.
Further testing could include more imaging tests, such as a heart MRI or CT scan. More invasive testing with cardiac catheterization might be used to measure how strongly your heart pumps and to scrutinize for blood vessel blockages.
Treatment
Medication. Two groups of medications called beta blockers and ACE inhibitors are primarily used to treat cardiomyopathy. “Those are very effective and they’re mainstays,” Douglas says. Medications help the body avoid overcompensating for heart dysfunction, she explains. Other types of drugs may also be used.

ACE inhibitors. Angiotensin-converting enzyme inhibitor medications like enalapril (Vasotec) widen blood vessels to increase blood flow in the heart.
Beta blockers. Medications such as metoprolol (Lopressor and Toprol XL) and carvedilol (Coreg) reduce the heart’s workload and prevent further heart damage.
Diuretics. Diuretics, or “water pills” like furosemide (Lasix), help eliminate excess fluid that can cause shortness of breath and swelling.
Digoxin. In some types of cardiomyopathy, digoxin can strengthen the heart’s ability to pump blood.
Also read: Macular Degeneration : A Patient’s Guide To Macular Degeneration And Its Symptoms
images source: Google
Disclaimer: The opinions and suggestions expressed in this article are solely those of the individual analysts. These are not the opinions of HNN. For more, please consult with your doctor.