Know the basics of symptoms, diagnosis, and treatment to help you deal with this cervical cancer.
In the U.S., an estimated 13,200 women are newly diagnosed with invasive cervical cancer in a single year. Cervical cancer claims the lives of about 4,250 women a year, according to the latest figures from the American Cancer Society.
When detected early, it is considered highly treatable and curable. Fortunately, with routine screening, earlier-stage cervical cancers are more commonly discovered than more-advanced, later-stage cervical cancers.
Also read-Brain cancer : A Patient’s Guide to Brain Cancer
All ages of women are vulnerable. The Centers for Disease Control and Prevention state that 49 years old is the average age at which it is diagnosed. However, women in their 20s may develop it.
What is cervical cancer?
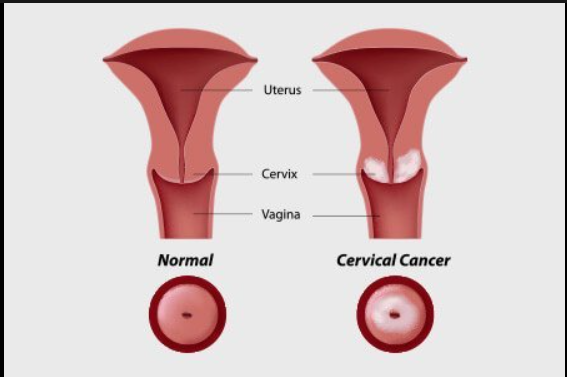
Cervical cancer is a cancer of a woman’s reproductive system. The cervix is the lower, narrower part of the womb, or uterus. The cervical opening connects the uterus to the vagina.
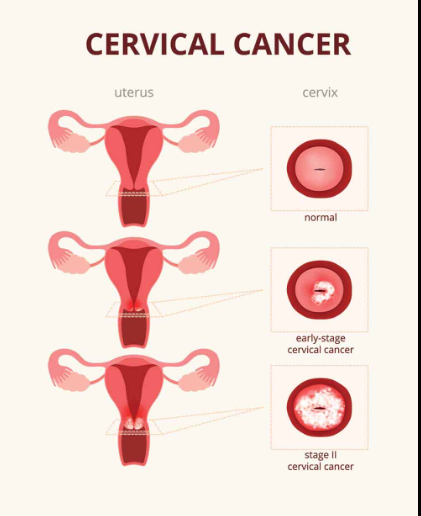
In cervical cancer, healthy cells of the cervix undergo genetic changes, or mutations. These abnormal cells grow out of control and form tumors. Precancerous changes in the cells, called dysplasia, can slowly develop over many years. If caught in time, they can be removed.
Cervical cancer is most often caused by the human papillomavirus, or HPV. Infection with HPV, which usually occurs through sexual contact, is common in men and women alike. Typically, the body’s immune system clears the virus on its own. In a minority of women, however, certain types of HPV may persist and cause cancerous changes in the cervix.
Up to 90 percent of cervical cancers are squamous cell cancers, based on the type of cervical cells in which they originate. Other cervical cancers, called adenocarcinomas, develop from gland cells within the cervix.
Pap tests, also called Pap smears, detect precancerous changes or cancerous cervical cells. A different screening method uses HPV testing. A positive HPV test reveals that you have an HPV-virus type that may be linked to cervical cancer.
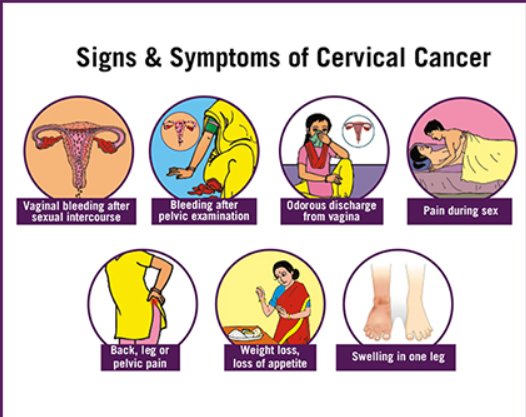
Signs and symptoms
“Abdominal or pelvic pain, watery or malodorous vaginal discharge, and irregular or dysfunctional vaginal bleeding are classic signs of cervical cancer,” says Dr. Amanda Fader, director of the Center for Rare Gynecologic Cancers at Johns Hopkins Hospital in Baltimore and the Kelly Gynecologic Oncology Service.
“Many of the cervical cancer lesions, or masses, start on the external surface of the cervix that protrudes into the vagina,” says Fader. “With sexual intercourse and penetration, that can cause a little disruption of the lesion or tumor, and that can present with abnormal bleeding.”
If you experience any of these symptoms, consult your primary care physician or gynecologist. After obtaining your medical history, your doctor will conduct a physical examination. According to Fader, the examination includes a sterile speculum in addition to a bimanual, or two-handed, examination of the cervix, vagina, and rectal regions.
When women raise concerns about abnormal discharge or spotting after sexual activity, it’s critical for physicians to pay close attention and follow up with additional information, advises Dr. Jennifer Mueller, a surgeon at Memorial Sloan Kettering Cancer Center in New York City who specializes in treating women with gynecologic cancers.
Even if you feel fine, you should periodically undergo a careful physical exam, including visualization of the cervix. “Sometimes a woman can have a completely normal Pap smear but an obvious lesion on the cervix,” Mueller says. “You should biopsy that. Pap smears are not 100 percent sensitive and specific tests; they’re screening tests.”
Diagnosis
Women evaluated for possible cervical cancer may go through a process like this:
- Symptoms like spotting or abnormal vaginal discharge raise concern.
- A doctor’s office visit includes a detailed history and a thorough gynecological exam.
- A screening test like a Pap smear reveals unusual or abnormal cells.
- Colposcopy—an exam of the cervix, vagina, and vulva using a special scope—is performed.
- A biopsy of tissue from the cervix and surrounding areas is done, if indicated.
- In the laboratory, cancer cells are found under the microscope.
In some cases, Mueller says, imaging tests used for a different reason, for instance, during an emergency room visit, might unexpectedly show a lesion on a woman’s cervix.
Stages
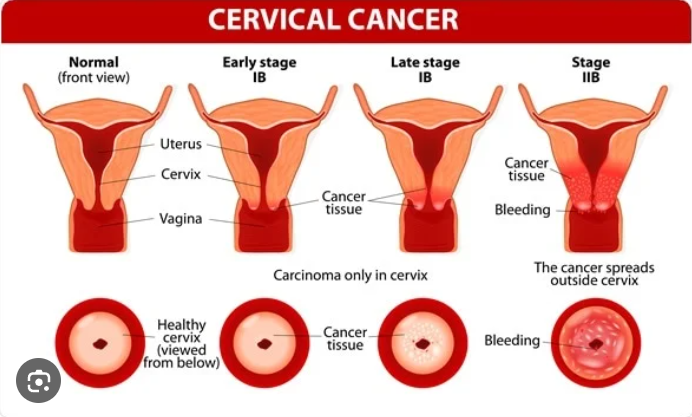
Once cervical cancer is diagnosed, CT scans, X-rays, MRIs, positron emission tomography, or PET scans help reveal its extent. Imaging can show whether cancer has spread outside the cervix.
Cervical cancer is broadly classified into four stages. Precise levels exist within stages, depending on tumor size and other features.
Stage 1 cervical cancer is limited to the cervix. Stage 2 cervical cancer is also seen in nearby areas of the vagina but is still confined to the pelvis. Stage 3 cervical cancer has spread to the pelvic wall and may affect the kidneys.
Stage 4 or late cervical cancer has spread to other parts of the body, including nearby areas like the rectum or distant organs such as the liver, bones, or lungs. Cancer may also have spread to the lymph nodes. Recurrent cervical cancer has returned to the body after previous treatment.
Treatment
The primary treatment for cervical cancer in its early stages is surgery. Your treatment team will go over the pros and cons of surgery with you if you have Stage 1 cervical cancer. While choosing a course of treatment, take your desired level of fertility into account.
“Depending on whether the woman desires future fertility, there are different types of procedures that can be performed in order to treat the cancer,” says Fader. If the cancer is detected early enough in its course, some of them may be uterine-sparing. Nonetheless, a hysterectomy or a radical hysterectomy is the usual treatment for early-stage cervical cancer.”
In a simple hysterectomy, the cervix and uterus are removed. In radical hysterectomy, part of the vagina and nearby lymph nodes are also removed, along with the cervix and uterus. A hysterectomy can be performed as a traditional open surgery involving an abdominal incision.
Minimally invasive surgery, by contrast, is done using a laparoscope, with specialized surgical tools inserted via tiny incisions. Robotic-assisted laparoscopy is one type of laparoscopic surgery.
Also read-Two Uteruses, Two Babies: A Single Woman’s Story Of Two Uteruses And Two Babies
images source: Google
Disclaimer: The opinions and suggestions expressed in this article are solely those of the individual analysts. These are not the opinions of HNN. For more, please consult with your doctor.