Your guide to causes, symptoms, treatments, and more for GERD
Have you ever felt as though your heart was on fire? This is something that many of us experience, particularly after a large, spicy meal or right before bed. This feeling, known as heartburn, will typically go away on its own or with the assistance of an antacid tablet purchased over-the-counter.
While heartburn is a rare occurrence for most of us, it can become a much more frequent issue for others. Individuals who frequently experience heartburn may have gastroesophageal reflux disease.
Also read-Constipation : A Patient’s Guide To Constipation And Its Symptoms
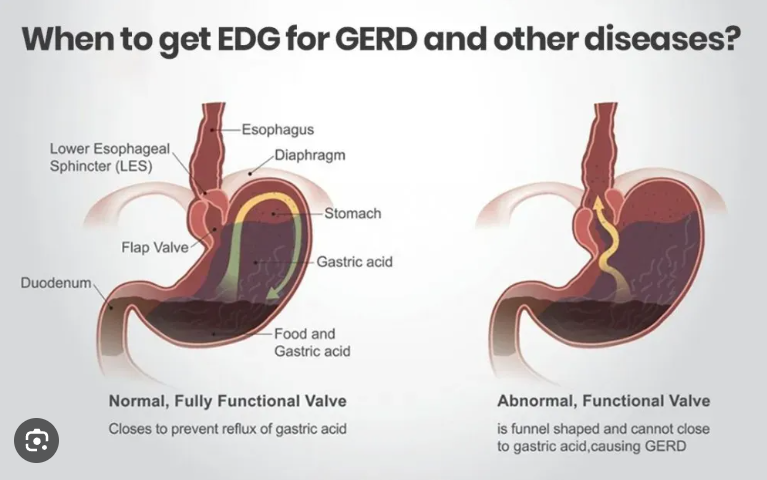
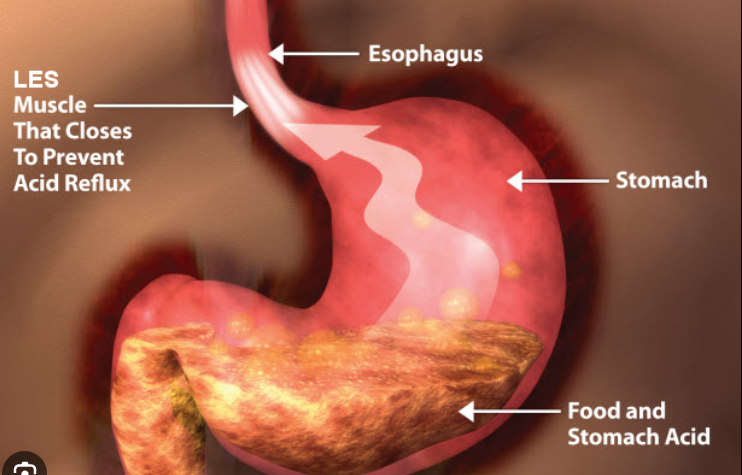
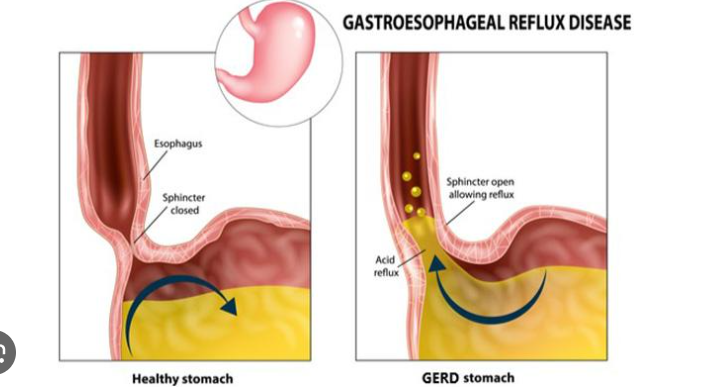
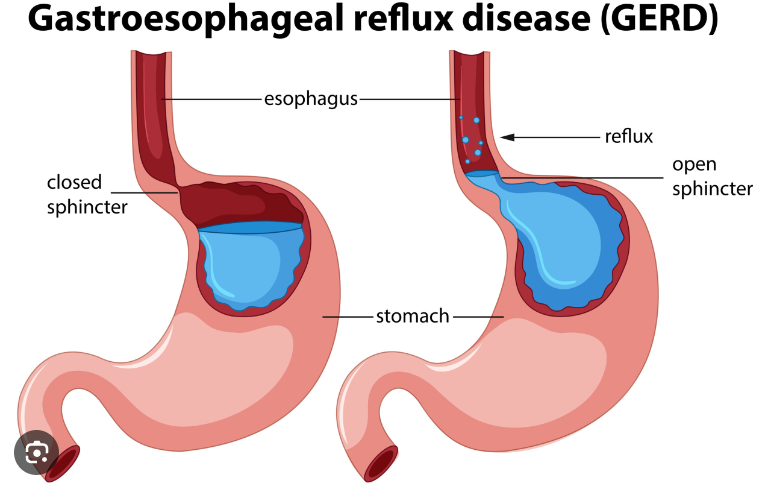
What is GERD?
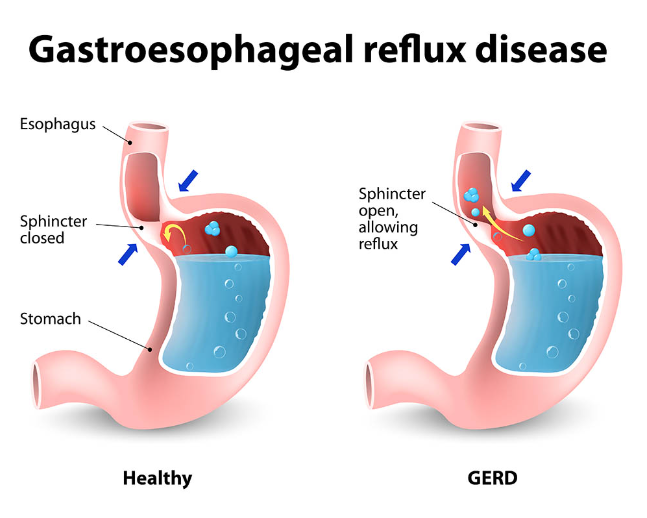
According to gastroenterologist Dr. Scott Gabbard of the Cleveland Clinic in Ohio, “GERD is a disorder where stomach contents come back up through the lower esophageal sphincter, which is the lower valve of the esophagus.” The lower esophageal sphincter allows the stomach’s contents, which can include food, stomach acid, and enzymes, to escape and cause issues in the esophagus. In actuality, GERD is a valve disorder in which the lower esophageal sphincter opens when it shouldn’t.”
As per the National Institute of Diabetes and Digestive and Kidney Diseases, physicians may also address the illness under several other titles, such as:
- Acid indigestion.
- Acid reflux.
- Acid regurgitation.
- Heartburn.
- Reflux.
GERD is a very common problem in the United States. The American College of Gastroenterology reports that “more than 60 million Americans experience heartburn at least once a month and some studies have suggested that more than 15 million Americans experience heartburn symptoms each day.” Simple heartburn becomes GERD when it happens two or more times per week.
“Up to 20 percent of the U.S. population has GERD, depending on which study you read,” Gabbard says. “So, it’s actually very common for the valve to open when it’s not supposed to,” and in fact, even in healthy patients who have no symptoms, it’s normal for reflux to occur for up to an hour per day, he says.
Causes and risk factors
There are lots of factors that can go into the development of a case of GERD, but some of the most common include:
- Diet. “Eating fatty meals triggers the valve to open more,” Gabbard says. It’s believed that this occurs so that you’ll be able to accommodate more food, as happens when taking in a large meal. “If you’ve eaten a large meal, there’s some sort of nerve signaling that’s probably mediated by nitric oxide. That allows the muscle to relax” and allows the valve to open more easily. “Theoretically, these high-fat meals trigger more nitric oxide release, which then allows the sphincter to open. It’s probably a trait that has evolved to allow people to belch so they don’t feel so much pain after eating a large meal.”
- Being overweight. Gastroenterologist Dr. Lisa Lih-Brody, M.D., of ProHealth Care in New York City, claims that part of the reason GERD incidence is rising in America is the country’s growing weight problem. Regretfully, GERD is becoming a more serious issue in the US. The increasing weight of the population in America is one of the main causes of this. The obesity epidemic is brought on by an increase in the average weight. One risk factor for reflux is obesity, according to her.
- Age. GERD is more common among adults over age 50. Over time, the elasticity of the esophageal sphincter declines, and that can lead to it opening when it shouldn’t. “Some studies suggest the valve becomes leakier as you age and doesn’t quite work as well as you get older,” Gabbard says.
- Sex and race. Caucasian men are more likely to get GERD.
- Pregnancy. The simple fact of accommodating a baby in your belly can cause crowding among your internal organs and for some women, this means the development of GERD because stomach contents have nowhere else to go but up.
- Frequent use of nonsteroidal pain relievers. Over-the-counter medications like ibuprofen (Advil, Motrin) and naproxen sodium (Aleve) can cause inflammation in the upper gastrointestinal tract, which can trigger or exacerbate symptoms of GERD.
- Having a hiatal hernia. A hiatal hernia occurs when the top part of the stomach pushes through the diaphragm muscle and balloons into the chest cavity. This can force stomach contents where they don’t belong, leading to symptoms of GERD.
- Smoking. Using tobacco is also considered a risk factor for GERD.
Symptoms
“A burning sensation in the center of the chest that usually occurs after a meal or when the patient lies down at night is the first typical symptom of GERD,” says Gabbard. Regurgitation is the second-most common symptom. Even though there might not be any burning, you will feel as though food is entering your stomach and entering your mouth and throat.”
In addition, Lih-Brody notes that GERD can also manifest as “burning in the upper part of the stomach radiating into the chest, burping, nausea, a feeling of fullness or of getting full quickly”. “Rarely you can have extra esophageal manifestations such as a sore throat, hoarse voice, pneumonia and a cough.” These are less frequent signs that may indicate further issues are present.
Diagnosis
If you’re experiencing frequent heartburn, it may be time to see your doctor, particularly if you have any so-called “alarm symptoms,” such as bleeding, weight loss and anemia, which may signal the presence of ulcers or strictures. “Unintentional weight loss, signs of bleeding, such as black tarry stools and if you’re having profound vomiting – these are alarm symptoms that should prompt someone to visit a physician. Also, if the heartburn and regurgitation becomes a regular and bothersome symptom, then clearly they need to visit the physician,” Gabbard says.
Treatment
“In 2019, there’s still no FDA-approved medicine that helps prevent the valve from opening,” Gabbard says, so “all of our therapies stop the stomach from making acid.” A class of drugs called proton pump inhibitors, such as omeprazole (Prilosec), esomeprazole (Nexium) and lansoprazole (Prevacid) all reduce the amount of acid manufactured in the stomach. “The problem is you still have the valve opening and the contents coming back up, but there’s no acid in that content, so patients don’t feel it,” Gabbard says. Therefore, in general, “provided that a patient doesn’t have any alarm features, our typical first-line approach would be a proton pump inhibitor to prevent the stomach from secreting acid.” For many patients, simply reducing the stomach acid takes care of the symptoms.
While some of these medications are available over the counter, Lih-Brody warns against simply reaching for a drugstore remedy, even if you’re pretty sure you’re dealing with GERD. “See a doctor. Don’t just self-medicate. That’s the true danger. A lot of the proton pump inhibitors are over-the-counter medications and people are just taking them willy-nilly. That’s dangerous because you could be sitting on a brewing ulcer, Barrett’s esophagus or esophageal cancer. Seeing a doctor sooner could have prevented the whole thing.”
Gabbard agrees that as soon as symptoms begin to impact your life, you should seek care. “If the regurgitation is a regular and bothersome phenomenon where it’s affecting quality of life, that’s clearly a time to see a physician, because reflux can turn into some bad things. When you have acid reflux some of the serious conditions can arise.”
In addition to medications, lifestyle modifications will likely be part of your treatment plan, too. Lih-Brody says that for many patients, this means avoiding foods that trigger GERD. “We tell people to stay away from irritants to the GI tract,” which are commonly thought to include such treats as chocolate, peppermint, spearmint, carbonated beverages, alcohol and fatty foods. “But Americans like to eat things like that, and unfortunately the reflux situation has become an epidemic.”
Also read-Osteoporosis : A Patient’s Guide to Osteoporosis
images source: Google
Disclaimer: The opinions and suggestions expressed in this article are solely those of the individual analysts. These are not the opinions of HNN. For more, please consult with your doctor.



































