Are you concerned about your blood sugar levels while you’re pregnant? Learn all about gestational diabetes, including how to prevent it, warning signs to watch for, and how to treat and manage it.
Certain women experience elevated blood sugar levels during pregnancy, which may pose a risk to both the mother and the fetus. According to the Centers for Disease Control and Prevention, gestational diabetes—a form of diabetes that develops during pregnancy—affects between 2% and 10% of pregnancies.
Also read-HIV/AIDS : A Patient’s Guide To HIV/AIDS And Its Symptoms

What’s gestational diabetes?
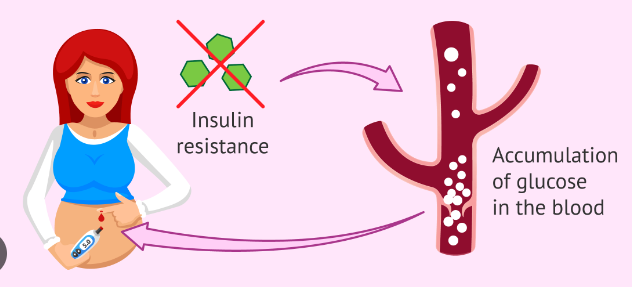
The body produces unique hormones and experiences other changes, such as weight gain, during pregnancy, which impact the cells’ capacity to utilise insulin and exacerbate insulin resistance. Even though most pregnant women can produce enough insulin to overcome insulin resistance, all of them experience some level of it in the latter stages of their pregnancy. Some, however, are unable to. Gestational diabetes strikes these women, usually detected by routine screening between weeks 24 and 28 of pregnancy.
What causes gestational diabetes?
The condition occurs when the body isn’t able to make enough of the hormone insulin, which helps regulate blood sugar. Changes during pregnancy, such as an increase in hormone production and weight gain, can cause insulin resistance, leading the body’s cells to use insulin less effectively. More insulin is needed as a result.

The reasons some women develop gestational diabetes aren’t fully understood, but there do appear to be some factors that can increase your risk of developing the condition.
Risk factors:
- Being overweight.
- Family history of type 2 diabetes.
- Previous pregnancy with a diagnosis of gestational diabetes.
- I gave birth to a baby weighing over 9 pounds.
- Are more than 25 years old.
- Have a hormone disorder called PCOS.
- Are an African American, Hispanic or Latino, American Indian, Alaska Native, Native Hawaiian, or Pacific Islander person.
Symptoms of gestational diabetes
It’s common for there to be no overt signs of gestational diabetes. If you do have symptoms, they may be mild, such as:
- Being thirstier than normal.
- Requiring you to urinate more often.
- Being more tired than usual or feeling extra-tired after eating.

“Women that are spiking blood sugars after they eat carbohydrate-laden meals are more likely to come crashing down two or three hours after they’ve had a meal and feel extremely tired, sluggish, and gain weight faster,” says DeVeciana Haugh. But it’s hard to distinguish those symptoms from other normal changes during pregnancy.
As is the case for others who may be developing Type 2 diabetes, those with gestational diabetes also have a tendency to need to urinate more frequently. “Polyuria, or the tendency to urinate more frequently, is one of the classic symptoms,” according to DeVeciana Haugh. However, many expectant mothers will tell you, “Well, I urinate all the time anyhow.”
Most of the time, women with gestational diabetes don’t show any symptoms. Other types of diabetes have more overt symptoms, such as frequent urination or thirst, according to Dr. Kelli Culpepper, an OB-GYN in private practice in Dallas and a Medical City Dallas Hospital affiliate. “Those things don’t happen in gestational diabetes,” she claims. The absence of external signs characteristic of GDM is all the more reason why experts emphasize the importance of routine screening.
How gestational diabetes diagnosed?
Screening is now almost universal because even evaluating known risk factors for gestational diabetes misses many who go on to develop it. As gestational diabetes usually manifests around week 24, you should anticipate being tested between weeks 24 and 28 of your pregnancy.
“Almost everyone is screened unless they have no risk factors for gestational diabetes, and almost everyone in the United States has some risk factors for diabetes,” says Dr. Ellen Seely, a professor of medicine at Harvard Medical School and director of clinical research, endocrinology, diabetes, and hypertension at Brigham and Women’s Hospital in Boston.
Those who are at higher risk, based on a family history of diabetes or other factors, may be advised to get tested earlier, during the first visit after becoming pregnant.
There’s ongoing debate over the best approach to testing: Some experts say performing a single gestational diabetes test is the best way to check for the condition. Most providers in the U.S. currently use a two-test system, which is endorsed by the American College of Obstetricians and Gynecologists
Treatment of gestational diabetes
The ultimate goal is always to have a healthy pregnancy, which is definitely within reach for any woman who has been diagnosed with gestational diabetes.

Beyond just preventing it, healthy eating, regular exercise, and maintaining a healthy weight can all help a woman reduce her risk of developing gestational diabetes.
Diet and physical activity
“Any lifestyle modification that improves a woman’s health prior to pregnancy is going to lessen her risk of developing diabetes when she gets pregnant—or, if she does get diabetes, improve her chances of being able to control it with just diet and exercise rather than having to take a medication for it,” DeVeciana Haugh says.
In fact, for many women with gestational diabetes, lifestyle changes alone are sufficient to manage blood sugar.
Checking blood sugar
Together, you and your diabetes educator will monitor your blood sugar levels throughout the day. Typically, this is done in the morning and right after meals using a finger stick. Instead of repeatedly puncturing a finger to take blood, there are diabetes patches, also known as flash glucose monitors, that allow you to continuously check your blood sugar levels. You wear a tiny patch sensor on your arm.
“It does have a tiny needle that goes just under the skin; then you don’t have to prick your finger for blood sugars; you just swipe a sensor in front of it,” says Philis-Tsimikas. It lasts for ten days before needing to be changed out for a new patch sensor.
Whatever approach you take, clinicians remind us that there are plenty of reasons to properly control GDM. When it’s not well managed, along with an increased likelihood of developing pre-eclampsia, women have a greater chance of delivering a bigger baby, which can increase the risk for childbirth-related injury to mother and child.
Medication
In some cases, patients may require insulin injections if lifestyle changes alone aren’t enough to bring down blood sugar levels. (Medications like metformin are sometimes prescribed as an alternative to insulin, though research supports insulin as the first choice.)
Also read-Skin Cancer : A Patient’s Guide To Skin Cancer And Its Symptoms
images source: Google
Disclaimer: The opinions and suggestions expressed in this article are solely those of the individual analysts. These are not the opinions of HNN. For more, please consult with your doctor.