Although they are not common, gluten sensitivities are quite real. See if you have this allergy by looking at these typical symptoms and additional potential reasons.
Is gluten really the culprit?
Consuming gluten, a protein present in wheat, barley, and rye, can cause damage to the small intestine in people with celiac disease. The symptoms of celiac disease might vary. Dr. Benjamin Lebwohl, an associate professor of medicine and epidemiology at the Columbia University Irving Medical Center in New York City, states that they can include intestinal problems such as nausea, vomiting, diarrhea, bloating, and abdominal discomfort. They can also include unintended weight loss and iron deficiency.
Also read–Quick Constipation Relief: How To Go To The Bathroom On Your Own
This is on top of other issues like exhaustion, mood swings, rashes, joint discomfort, cognitive symptoms (often referred to as “brain fog”), numbness and tingling in the extremities, and so forth. Sensitivity after consuming it However, while weight loss and nutritional deficits are linked to malabsorption from intestinal damage found exclusively in cases of true celiac disease, those symptoms typically don’t include them. Experts explain that because it can cause such a wide range of symptoms, people tend to blame it for everything when, in reality, it may not be the cause. Prior to deciding to go gluten-free, think about other possible reasons for your symptoms.
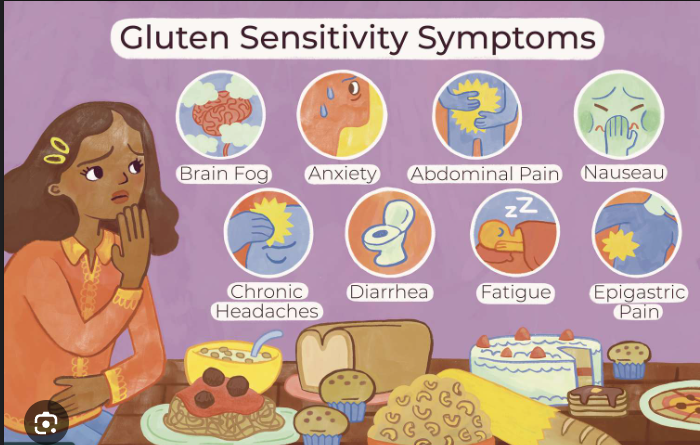
Gluten intolerance symptoms checklist
These are symptoms of possible intolerance:
- Abdominal pain.
- Bloating.
- Gas.
- Diarrhea.
- Constipation.
- Nausea and vomiting
- Anxiety or depression.
- Fatigue.
- Brain fog.
Could something else be causing your symptoms?
It is possible, theoretically, to have a wheat-specific issue (like a wheat allergy), but not a gluten-specific one, as it may be found in grains like barley and rye that don’t contain wheat. The general term “non-celiac gluten sensitivity,” which is used to refer to a sensitivity to it in people who do not have celiac disease, is even up for debate among researchers and clinicians. Some argue that it should be renamed wheat intolerance syndrome or something else entirely.
Celiac disease vs. NCGS
There are tests that can help distinguish celiac disease from illnesses that mimic it.
The director of the UCLA Celiac Disease Program and an assistant professor of medicine in the division of digestive diseases at the David Geffen School of Medicine at UCLA, Guy A. Weiss, explains that “celiac disease is an autoimmune condition, affecting about 1% of the population, in which the immune system is triggered in response to gluten exposure, leading to gut inflammation.” “Diagnosis is based on typical small bowel biopsy findings and elevated celiac-associated antibodies found in blood tests.”
With non-celiac sensitivity, the diagnosis is less clear-cut. “NCGS is not a well-understood syndrome,” says Weiss, who is the editor of “Diagnosis and Management of Gluten-Associated Disorders: A Clinical Casebook.”NCGS, which affects an estimated 2% to 3% of people, “is diagnosed clinically after excluding celiac disease and wheat allergy in those with symptoms that are associated only with it exposure,” he says. “People with NCGS do not have the above-mentioned abnormal laboratory or biopsy findings.”
Cases of mistaken identity
Without the advice of a qualified dietitian nutritionist, eliminating it may have unforeseen health effects. According to Lebwohl’s research, which was published in the May 2017 issue of the journal BMJ, avoiding it in food may lead to a decrease in the intake of whole grains, which may raise the risk of cardiovascular disease. Furthermore, a prior study in which Lebwohl participated discovered that 25 out of 84 individuals who did not have celiac disease but claimed gluten was making them sick were given a variety of alternative diagnoses.

“The takeaway from that study is that just because a patient makes a connection between it and symptoms does not automatically mean that that patient has non-celiac sensitivity,” Lebwohl says.
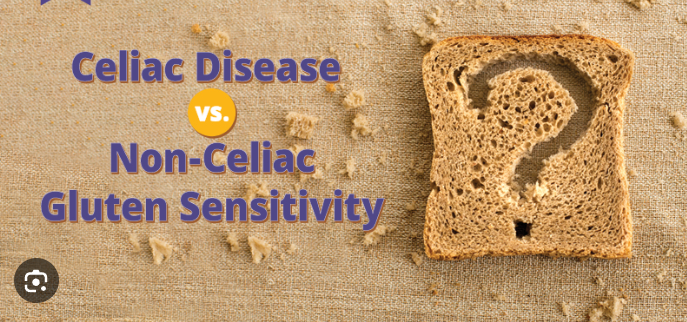
Added fiber, artificial sugars and alcohol
There is no shortage of foods that you might eat that could result in gastrointestinal issues, for which it is frequently blamed. This includes high concentrations of the fiber inulin (chicory root), as well as sugar-replacement additives like sorbitol, maltitol, and lactitol found in protein bars and other items like ice cream goods, which are also frequently poorly digested, according to Stefanski.
She continues, saying that eating too much or too little fried or high-fat food might cause digestive problems that are occasionally linked to gluten. “When alcohol is consumed in excess, it can cause diarrhea,” claims Stefanski. “Beer, which is made from barley and contains gluten, does cause reactions in certain people, but it isn’t always the cause.” Although wine often doesn’t contain gluten, it can cause problems as well.
How to navigate gluten intolerance
When it comes to stomach issues, resist the urge to go it alone. “It’s critical to work with a GI-dietitian and a doctor who is knowledgeable about gluten-associated disorders to manage diets like the gluten-free diet,” adds Weiss. “Inadequate diagnosis and strict avoidance can be harmful, increasing the risk of weight gain, diabetes, and osteoporosis and decreasing bone density.”
Digestive diseases can have hereditary tendencies, but genetic testing is more helpful with some conditions than others. “Although NCGS tends to DQ8in families, no predisposing genes have been detected, unlike the HLA DQ2 and DQ8 genes that are found in individuals with celiac disease,” Weiss says.
Reintroducing gluten?
Gluten in food doesn’t necessarily have to be outlawed in some situations.

According to Weiss, “We customize a gluten-free diet for each patient at the UCLA Celiac Disease Program based on their level of sensitivity to it.” “Those with NCGS are less sensitive to gluten exposure, in contrast to those with celiac disease, in which crumbs can cause symptoms.” It’s not always necessary to eliminate it because NCGS can be temporary. “Those with severe NCGS may choose to remain on a gluten-free diet indefinitely, but after a year or two, we will attempt to reintroduce gluten again,” he explains.
A variety of conditions or certain foods can produce symptoms similar to those of non-celiac gluten sensitivity.
- Wheat (not gluten) allergy.
- Celiac disease.
- Lactose or fructose intolerance
- Foods with inulin, artificial sugars, or alcohol.
- Fried or high-fat fare
- Small intestinal bacterial overgrowth.
- Gastroparesis.
- Irritable bowel syndrome and high-FODMAP foods
- Serious health concerns, such as depression and other mood disorders.
Also read–Fresh Herbs Vs. Dried Herbs: Which Is Better For Cooking
images source: Google
Disclaimer: The opinions and suggestions expressed in this article are solely those of the individual analysts. These are not the opinions of HNN. For more, please consult with your doctor.




































