Know the basics of symptoms, diagnosis, and treatment to help you deal with heart arrhythmias.
An irregular heartbeat, or one that beats more or fewer times than usual, is known as an arrhythmia. It’s possible that you have erratic heartbeats, but they’re harmless variations of heart arrhythmias.
On the other hand, a few arrhythmias raise the possibility of cardiovascular diseases like heart failure or stroke. A small percentage of arrhythmias pose a risk to life if left undiagnosed or untreated.
Also read-Coronary Artery Disease : A Patient’s Guide To Coronary Artery Disease And Its Symptoms
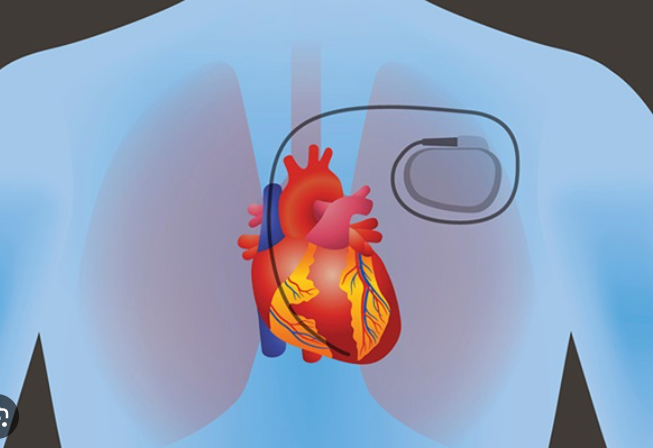
Heart implant devices may be necessary for patients with arrhythmias who are at the highest risk. Nonetheless, the majority of arrhythmias can be controlled with drugs or catheter insertions. You can have a normal life with appropriate care and regular safety measures.
What is an arrhythmia?
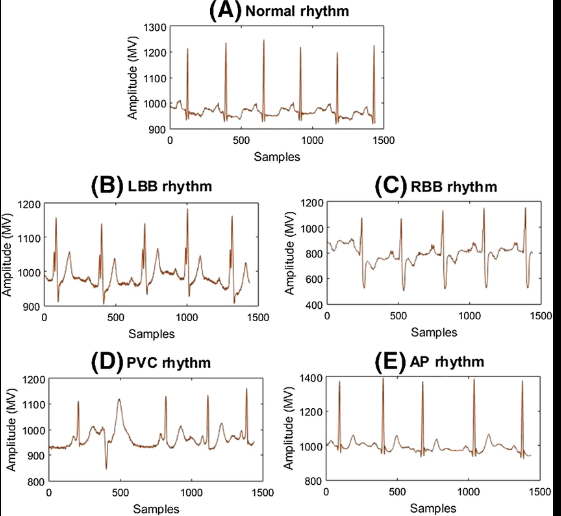
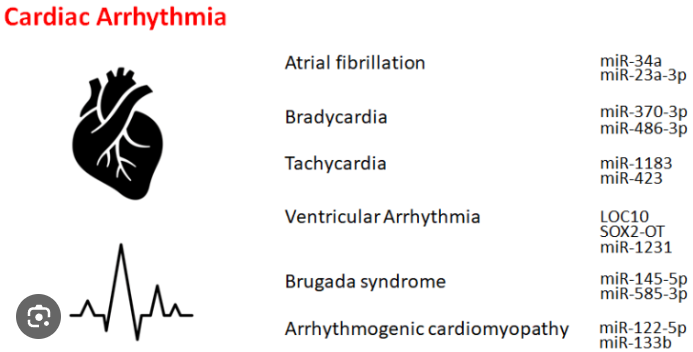
Heart arrhythmias are usually grouped in two ways. The first is by heartbeat frequency. A slow heart rate is called bradyarrhythmia. In general, a heart rate under 60 beats per minute is considered slow. A fast heart rate is called tachyarrhythmia—in general, above 100 beats per minute.
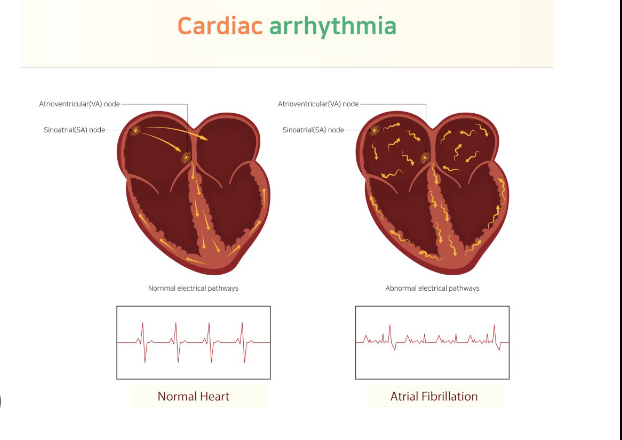
Arrhythmias can also be classified by the location in the heart where they originate. Supraventricular arrhythmias occur in the upper heart chambers, or atria, or in other cardiac structures.
Heartbeat: basics of heart arrhythmias
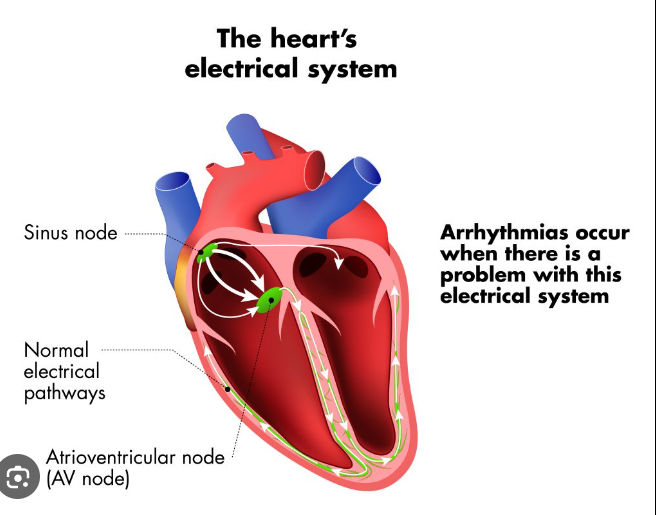
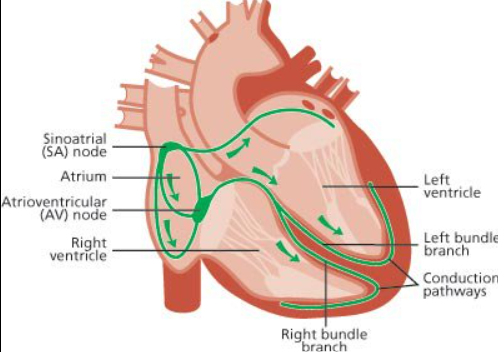
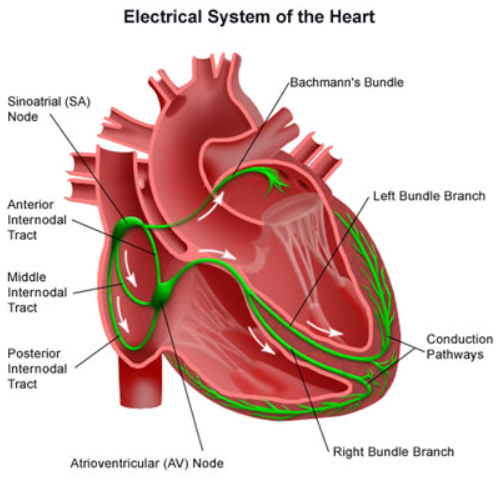
“The heart is a muscle and it’s a muscular pump,” says Dr. Joseph H. Levine, director of the Arrhythmia & Pacemaker Center at St. Francis Hospital in Long Island, New York. “Like any mechanical pump, electrical signals turn it on and off. In the heart, the electrical signals are built into the heart muscle itself. Every heart cell has the ability to have electrical activity that tells the individual cell to contract. The overall electrical system in the heart allows the contractions to be synchronous and organized.”
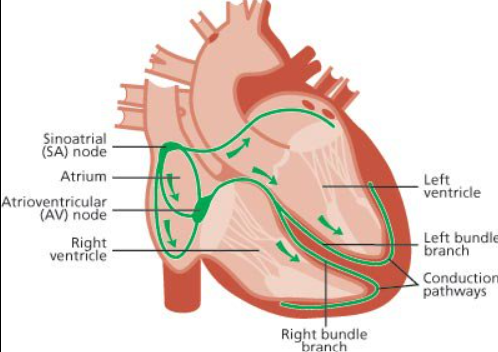
The natural pacemaker of the heart is the sinus node, which leads into the right atrium. The main electrical “wiring” of the heart is the atrioventricular node between the atria and ventricles.
The His-Purkinje system is responsible for rapid ventricular conduction. “This is specialized cardiac tissue that allows for very fast activity, so that all heart cells can simultaneously be activated to allow contractions to be synchronous,” Levine says.
When the heart doesn’t contract in an efficient, synchronized way, arrhythmia results.
Signs and symptoms of heart arrhythmias
Depending on your arrhythmia type or heart risk, you may experience the following symptoms:
Slow Heart Rhythm
- Fatigue.
- Syncope (fainting).
- Dizziness.
Fast heart rhythm
- Palpitations (feeling of a fast-beating or pounding heart).
- Lightheadedness or syncope.
- Shortness of breath on exertion.
- Anxiety sensation.
- Chest pain.
Causes of heart arrhythmias
Arrhythmias can result from heart or vascular conditions such as heart valve problems, high blood pressure, cardiomyopathy, or alterations in the heart’s muscle.
Childhood or adult congenital cardiac conditions, or birth defects such as the tetralogy of Fallot or atrial septal defect, can cause arrhythmias.
One of the most severe forms of fast arrhythmias can result from scar tissue in the heart, for example, following a heart attack. According to Dr. Vivek Reddy, who oversees the cardiac arrhythmia service at Mount Sinai Health System in New York City, “tachycardia circuits can develop.” “Ventricular tachycardia is dangerous; it’s actually the rhythm that leads to most cardiac arrests.”
In many cases, the cause of arrhythmia is unknown. One common misconception is that all arrhythmias are abnormal, Levine notes. For instance, a wearable fitness device may pick up a benign irregular heartbeat with no clear cause and no need for treatment. Premature ventricular contractions are early, extra heartbeats that start in the ventricles. PVCs are quite common and usually considered harmless unless people also have risk factors such as heart disease or heart failure. Premature atrial contractions, or PACS, are similar but start in the atria of the heart.
The cause may be external. “It turns out that caffeine causes a lot of arrhythmias,” Levine says. “Red wine causes a lot of arrhythmias. Alcohol excess causes a lot of arrhythmias, and the alcohol excess is called ‘holiday heart syndrome.’ You go on holiday and the next day you’re in the emergency room with arrhythmia.” For some people, limiting caffeine and alcohol may be enough to prevent future episodes.
Diagnosis of heart arrhythmias
To make an arrhythmia diagnosis, cardiologists ask patients about their medical history, perform a physical exam and order certain tests based on specific symptoms.
Tests to Diagnose Heart Arrhythmia
- An electrocardiogram is the primary diagnostic test. A 12-lead EKG is standard, Koplan says.
- A continuous wearable monitor, like a Holter monitor, is a small device that you wear around the clock for a day or two to catch arrhythmias that come and go. Wearable monitors can catch paroxysmal or nonsustained arrhythmias that an EKG may not pick up.
- Treadmill tests can help diagnose exercise-related arrhythmias.
- Echocardiograms are noninvasive ultrasound tests of the heart.
- Electrophysiology studies are done under local anesthesia, with cardiac catheters threaded into large blood vessels in the heart to determine the arrhythmia’s source.
Treatments of heart arrhythmias
If you have an arrhythmia that requires treatment, your cardiologist will explain your options and describe the risks and benefits of each one. Depending on your specific diagnosis, choices may include medications, catheter-based procedures, or implanted heart devices such as pacemakers and internal defibrillators.
Medications for Arrhythmia
Two main types of drugs are used to treat heart arrhythmia: anticoagulants and antiarrhythmics.
Anticoagulant drugs. “Blood thinners are used to prevent stroke for certain people who have atrial fibrillation and atrial flutter,” Levine says. Anticoagulants used to treat AFib include warfarin (Coumadin and Jantoven) and newer drugs such as Pradaxa (dabigatran), Xarelto (rivaroxaban), Eliquis (apixaban), and Savaysa (edoxaban).
Antiarrhythmic drugs. Certain types of oral medications prescribed to maintain a normal heart rhythm include the following:
- Sodium channel blockers to slow down the heart’s electrical signal include Norpace (disopyramide), Tambocor (flecainide), Rythmol (propafenone), and Quinaglute (quinidine).
- Beta-blockers like Toprol XL (metoprolol) slow down the heart rate.
- Potassium channel blockers such as Betapace (sotalol) and Tikosyn (dofetilide) act on the heart muscle to improve rhythm.
- Calcium channel blockers such as diltiazem (Cardizem) and verapamil (Calan) slow down a too-fast heart rate.
- Pacerone or Cordarone (amiodarone) is used to treat life-threatening ventricular fibrillation or ventricular tachycardia.
Also read-Heart Failure : A Patient’s Guide To Congestive Heart Failure
images source: Google
Disclaimer: The opinions and suggestions expressed in this article are solely those of the individual analysts. These are not the opinions of HNN. For more, please consult with your doctor.