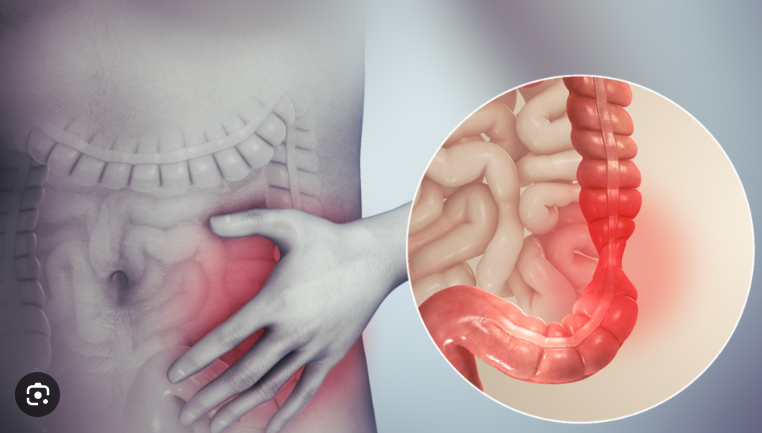
Constipation and diarrhea are possible signs of the brain-gut disorder of Irritable Bowel Syndrome
Constipation or diarrhea are uncomfortable conditions that everyone encounters occasionally. A simple case of constipation could be caused by eating too little fiber, whereas excessive use of laxatives or eating foods to which you are allergic could result in diarrhea or Irritable Bowel Syndrome
However, if you have chronic constipation, diarrhea, or both, you might have irritable bowel syndrome. One common intestinal disorder that affects many people is irritable bowel syndrome.
Also read-GERD : A Patient’s Guide To GERD And Its Symptoms
The director of the gastrointestinal motility lab at Massachusetts General Hospital in Boston, Dr. Kyle Staller, says that IBS arises from a communication breakdown between the brain and the gut.
Staller, an assistant professor of medicine at Harvard Medical School, says there isn’t a commonly used lab test to diagnose IBS. Instead, in order to diagnose the condition, clinicians use the Rome IV criteria. According to these criteria, an individual may have IBS if they have had recurrent abdominal pain and bowel movements at least once a week for the preceding three months.
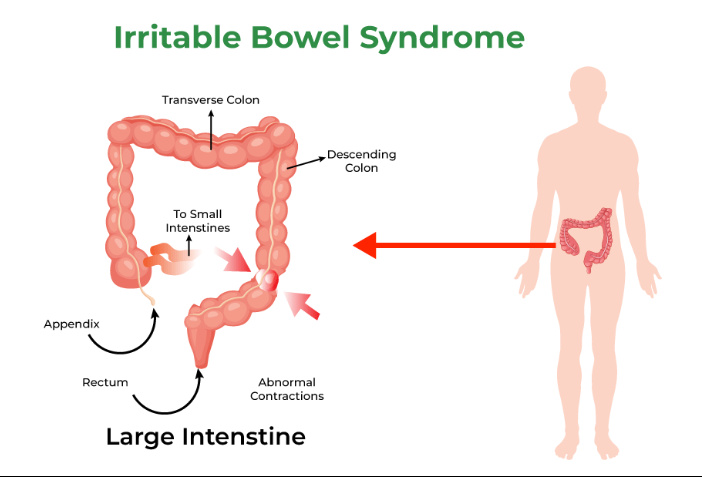
Causes of irritable bowel syndrome
It’s unknown exactly what causes irritable bowel syndrome, according to the Mayo Clinic.
These elements might be involved:
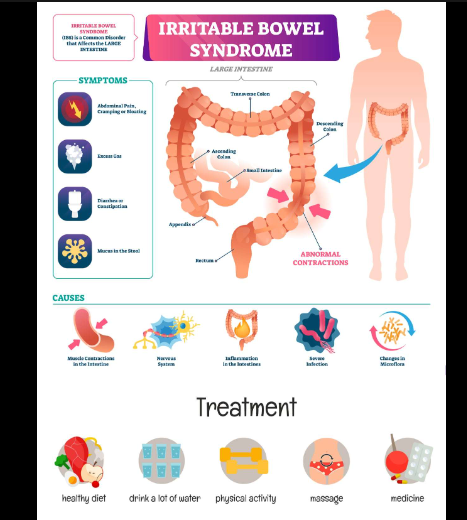
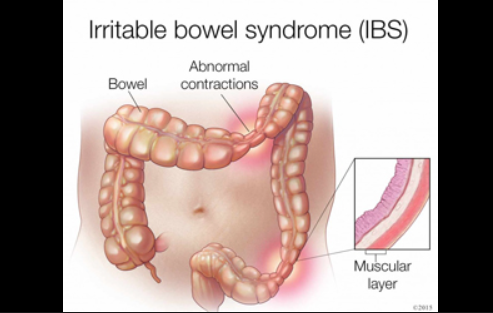
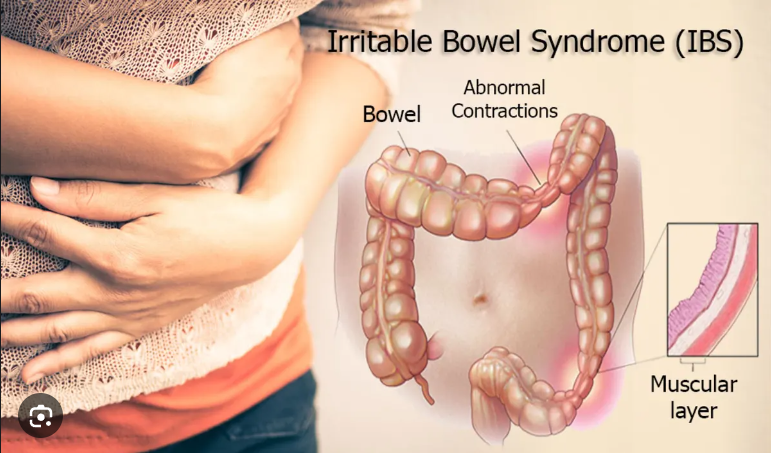
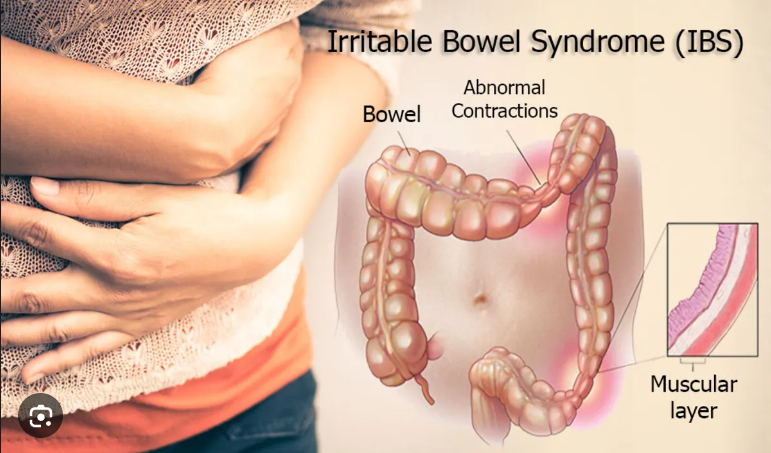
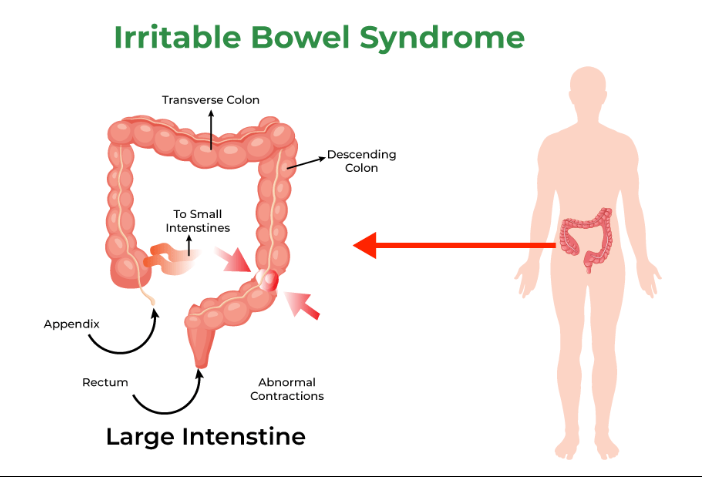
- contractions of the intestinal muscles. Layers of muscle that line the inside of your intestines contract to help food pass through your digestive tract. Bloating, diarrhea, and gas can result from contractions that are more intense and prolonged than usual. On the other hand, weak intestinal contractions may result in hard, dry stools.
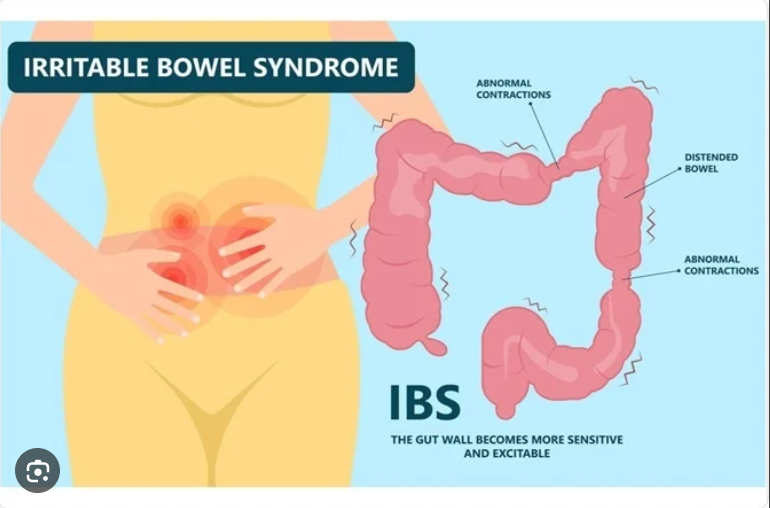
- Anomalies of the nervous system When your abdomen stretches due to the presence of gas or stool, abnormalities in the nerves supplying your digestive system may cause more sensitivity or discomfort than usual. Your body may overreact to normal changes in the digestive system if there is an imbalance in the signals that are sent from the brain to the intestines.
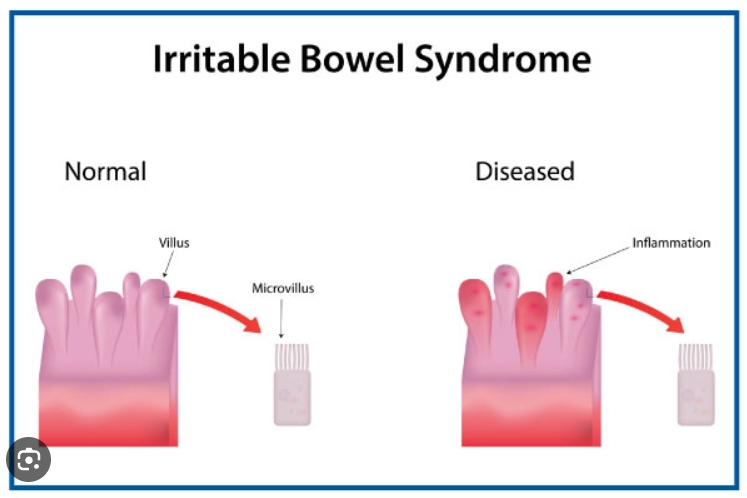
- An intestinal inflammation. There are more immune system cells in the intestines of some IBS sufferers. The immune system’s reaction is linked to diarrhea and pain.
- Severe infection. After a severe episode of diarrhea (gastroenteritis) brought on by a virus or bacteria, IBS may develop. An excess of bacteria in the intestines may also be linked to IBS.
- Alterations to the gut’s microflora, or bacteria The microflora that live in the intestines are referred to as “good bacteria,” and they are essential to good health. According to research, the microbiota of individuals with IBS may not be the same as that of healthy individuals.
Signs and symptoms
IBS signs and symptoms include:
- Constipation.
- Diarrhea.
- Alternating constipation and diarrhea
- Adominal pain or cramps.
- Mucus is in the stool.
- Gas and bloating.
It’s important to keep in mind that these symptoms could be from IBS, but they could also be associated with a host of other conditions, says Dr. Hardeep M. Singh, a gastroenterologist with St. Joseph Hospital in Orange, California.
Those conditions include colon cancer, colitis, Crohn’s disease or infection.
If you’re starting to experience these symptoms, you should be evaluated by a health care professional, Singh says.
Risk factors
There are no known risk factors for IBS, which occurs in about 10% to 15% of the U.S. population, Singh says. The occurrence of IBS peaks in people between the ages of 18 and 40, Singh says, adding that it can occur at any stage of life.
GI tract infections can be risk factors, but not everyone who experiences a GI infection will get IBS, Staller says.
Irritable bowel syndrome tends to be more common in patients with a history of:
- Anxiety.
- Depression.
- Fibromyalgia.
- Chronic fatigue syndrome.
Triggers
The symptoms of IBS can be triggered by a number of factors, including:
- Taking a strong course of antibiotics
- Following a bout of infectious gastroenteritis.
- Significant narcotic pain medication exposure.
- Eating certain foods.
“Significant pain medication exposure can slow the colon’s ability to move and function,” Lee says.
Diet
Consuming certain foods can trigger symptoms of IBS.
Foods that can trigger IBS include:
- Dairy products.
- Breads and cereals made with refined grains
- Processed foods, like cookies and snack chips.
- Coffee.
Diagnosis
There’s no lab exam, like a blood test, that can diagnose IBS.
“IBS is a diagnosis of exclusion,” Singh says. “Routine labs should be done to assess for signs of inflammation, bleeding, and infection. Other diseases should be ruled out, such as thyroid issues or celiac disease.”
Your health care provider may conduct certain tests to determine if your symptoms are caused by a condition other than IBS.
These tests could include:
- Endoscopy.
- CT scans.
- MRIs.
- Barium studies.
- Blood tests.
- Stool tests.
- Breath tests.
Treatment
There’s no cure for IBS, but there are a number of treatment approaches that can be effective in managing it, Singh says.
Treatment options include:
- Fiber. If constipation is an issue, consume more fiber.
- Anti-diarrheal medications. Some antispasmodic drugs can help alleviate diarrhea and cramps.
- Probiotics. These can sometimes help with gas, blotting, and diarrhea.
- Antibiotics. This type of medication can help some people with IBS who have “bad bacteria” in the gut, according to the International Foundation for Gastrointestinal Disorders.
- Stress reduction. Seeing a trained therapist or trying medications for depression or anxiety could help alleviate IBS symptoms for some people.
Also read-Scoliosis : A Patient’s Guide to Scoliosis And Its Symptoms
images source: Google
Disclaimer: The opinions and suggestions expressed in this article are solely those of the individual analysts. These are not the opinions of HNN. For more, please consult with your doctor.