Learn about the symptoms, causes, and treatment options for the different types of meningitis.
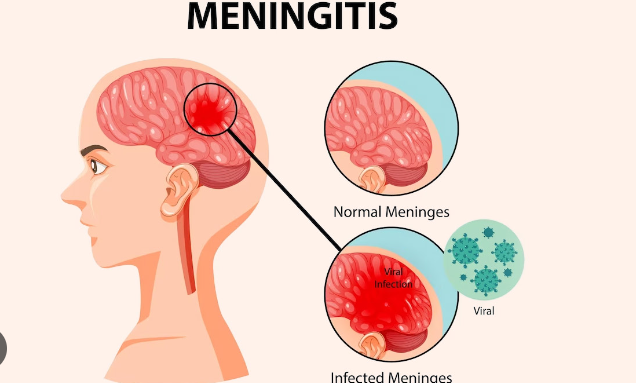
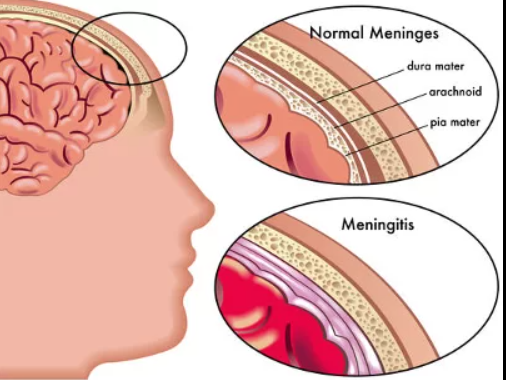
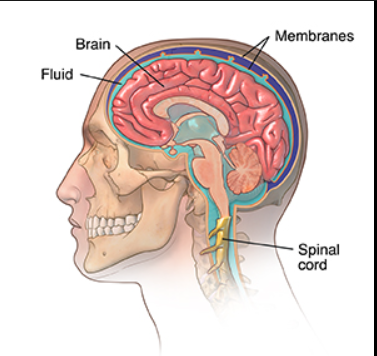
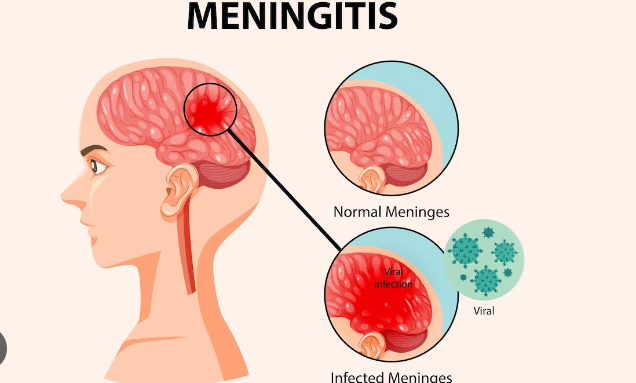
A broad term used to describe an inflammation affecting the membranes surrounding the brain and spinal cord is meningitis, specifically spinal meningitis. Meninges are the name for these membranes.
Spinal pain comes in a variety of forms, some of which are extremely dangerous or even fatal. Meningitis can also cause hearing loss, memory issues, developmental disorders, brain damage, seizures, arthritis, and limb loss. Cases are uncommon, though, since more vaccines are now available to prevent many types of pain. Viral and bacterial meningitis are the most prevalent types.
Also read-Epilepsy: A Patient’s Guide To Epilepsy And Its Symptoms
Spinal pain cases in the U.S. are at an all-time low, and doctors think that’s due to the increase in vaccinations for the disease. In 1989, for instance, there were 1.1 cases for every 100,000 people. As of 2017, that rate was only 0.11 per 100,000 people. Newborns and children under age 5 are at the highest risk for pain, followed by teens as the second-highest group at risk.
Types of meningitis
According to the Centers for Disease Control and Prevention, these are the various types of meningitis:
- Bacterial pain.
- Viral .
- Fungal .
- Amebic .
- Parasitic .
- Noninfectious .
Causes
There are different types of viruses and bacteria associated with spinal pain.

The most common viruses that cause viral pain include:
- Measles virus.
- Influenza virus.
- Mumps virus.
You can get these by coming into close contact with someone else who has the virus, but not everyone who comes into contact will get sick. It’s not always clear why some people get sick with viral pain after close contact and others don’t, says Dr. Amesh A. Adalja, a senior scholar with the Johns Hopkins Center for Health Security in Baltimore. “There may be genetic differences we don’t yet understand,” he says.
Similarly, bacterial pain is spread from one person to another. This is why vaccines are an important tool to keep the rates of bacterial pain low. The leading bacteria associated with bacterial pain in the U.S. are:
- Streptococcus pneumoniae.
- Group B Streptococcus.
- Neisseria meningitidis.
- Haemophilus influenzae.
- Listeria monocytogenes, which is spread through contaminated food.
Age usually determines which type of bacteria someone gets. For instance, the cause of meningitis in newborns is more likely to be from Group B Streptococcus, S. pneumonia, L. monocytogenes and the bacteria Escherichia coli, the CDC reports.
Risk factors
Newborns and children under age 5 are at a higher risk for certain types of meningitis than any other age group. This is because their immune system is not fully developed. Newborns and young babies also cannot state that they are in pain the way an older child or adult can. Newborns may contract certain types of bacteria causing meningitis from the birth canal

Traveling to an area of sub-Saharan Africa called “the meningitis belt,” or to Mecca during the annual Hajj pilgrimage, can increase the risk, according to the CDC. The risk is higher traveling to Mecca because of the millions of people grouped closely together who could easily pass infectious diseases. The CDC also notes that Saudi Arabia requires participants in the annual Hajj and Umrah pilgrimages show proof of meningococcal vaccination.
Symptoms
Viral and bacterial meningitis have similar symptoms including

- A sore throat.
- Fever.
- Headache.
- A stiff neck. Because the membranes around the brain and spinal cord are inflamed, it makes it difficult to bend the neck forward, Schaffner says.
- Feeling unusually tired or lethargic.
- A skin rash for certain types of meningitis.
These symptoms have some overlap with other common illnesses, like the flu, which may lead parents to worry if their child has meningitis. However, one key difference is the stiff neck.
“It’s painful to move the neck, and some can’t even move it. That’s not common with other infectious diseases,” Adalja says. If a doctor needs to determine if an infection is the flu versus meningitis, health providers can perform a rapid flu test, Clemens adds.
The extent of illness also is noticeable to family and friends. “It’s not subtle. The person who has this is clearly sick, and friends and family know they aren’t doing well,” Adalja says.
Because newborns can’t speak their symptoms like older children or adults can, signs to look out for include crankiness or a soft spot in the back of the head that is bulging. Babies also may have temperature instability, either becoming too hot or too cold, Clemens says.
If you suspect that you or someone you care for has meningitis, it’s important to see a doctor quickly for diagnosis and treatment.
Diagnosis
The main way that health providers diagnose meningitis is with a lumbar puncture, also called a spinal tap. This involves sticking a needle in the back to take out some of the cerebrospinal fluid. That fluid is then examined under a microscope to see if it’s consistent with infection.
A lumbar puncture has a similar feel to getting a shot – a bit painful, but not excruciating, Clemens says. In the emergency room, doctors often use local anesthesia over the skin where the puncture will take place. “Sometimes, it’s a nasty pinch. In my experience in the past, being held in a curled-up position (to complete a lumbar puncture) is what kids object to more than a poke,” Clemens says.
Other tests used for meningitis are a blood draw and imaging with computerized tomography (CT) or magnetic resonance imaging (MRI). However, the spinal tap is the most important clue in diagnosing meningitis.
Treatment
There is not much that doctors can do for viral meningitis except provide supportive care, says Dr. Stan Deresinski, a clinical professor of medicine for infectious diseases with Stanford Health Care in Menlo Park, California. Fortunately, with lots of rest, most people get better in a week to 10 days. Most patients with viral meningitis can rest at home and do not have to stay at a hospital. “It usually resolves, and a patient does fine without any residual effects,” Deresinski says.
Bacterial meningitis is more serious. “Left untreated, it is almost always fatal,” Clemens says. A person with bacterial meningitis will stay in the hospital to receive antibiotics intravenously and to monitor the signs and symptoms of meningitis, as the infection can quickly spread.
Antibiotics are the treatment used for bacterial meningitis, but the type of antibiotic varies depending on the type of bacteria found in each person. Until health providers know exactly what type of bacteria is causing meningitis, a person may receive a strong antibiotic that fights off a wide range of bacteria. Once the exact cause is known, the treatment might be changed to better target the patient’s illness, Clemens says.
Children with meningitis also may receive an early initial dose of corticosteroids to help reduce the inflammation, Deresinski says. Giving corticosteroids also can lower the risk of hearing loss that sometimes occurs after having bacterial meningitis.
Also read-Dementia : A Patient’s Guide To Dementia And Its Symptoms
images source: Google
Disclaimer: The opinions and suggestions expressed in this article are solely those of the individual analysts. These are not the opinions of HNN. For more, please consult with your doctor.