What you need to know about the causes, risk factors, treatment, and prevention of peptic ulcers
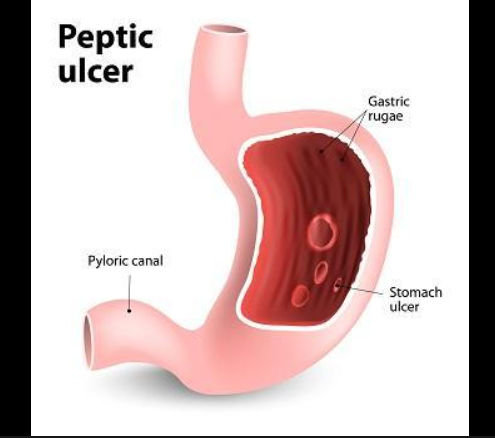
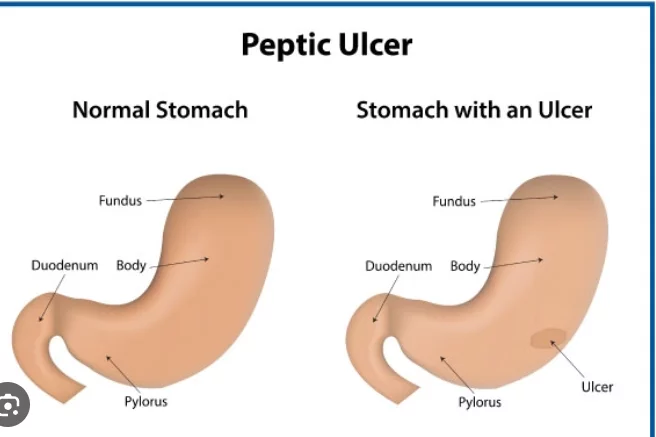
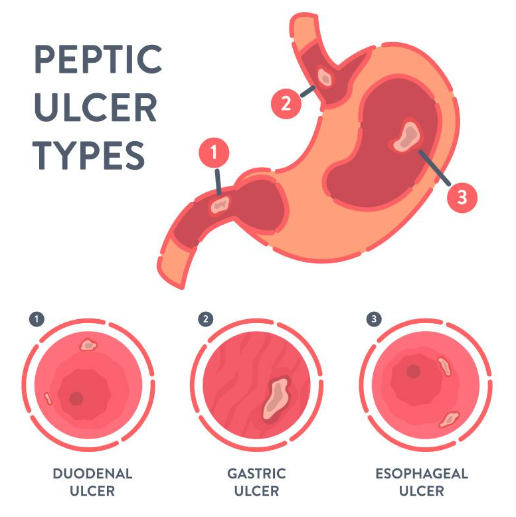
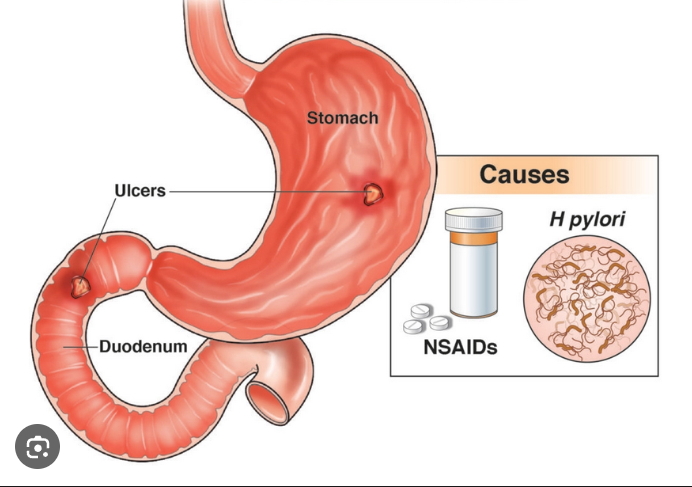
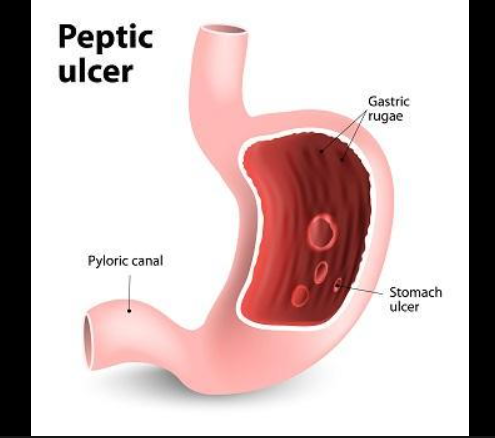
A partial hole or sore in the lining of your stomach or in the duodenum, a portion of your small intestine, is called a peptic ulcer. Depending on the location of the ulcer, your doctor may also refer to it as a duodenal or stomach ulcer.
One prevalent medical condition is peptic ulcers. According to Harvard Health, about 10% of Americans will at some point have one. About 4 million Americans suffer from peptic ulcers each year, which can strike anyone at any age.
Also read-Ulcerative Colitis : A Patient’s Guide To Ulcerative Colitis And Its Symptoms
Many peptic ulcer sufferers don’t even exhibit any symptoms. Others experience a variety of symptoms, such as upper abdominal pain, vomiting, and indigestion. On the other hand, some people with peptic ulcers only experience symptoms when they get really bad, like gastrointestinal bleeding or anemia from blood loss.
It’s critical to see a physician if you think you may have a peptic ulcer. Here is additional information regarding the signs, causes, complications, risk factors, diagnosis, treatment, and avoidance of peptic ulcers.
Causes of peptic ulcers
A peptic ulcer has two potential causes. The first culprit is a bacterium called Helicobacter pylori. This bacterium has developed ways to live in the acidic environment of the stomach, says Dr. Jesse P. Houghton, senior medical director of gastroenterology at Southern Ohio Medical Center Gastroenterology Associates in Portsmouth, Ohio. “The bacteria elicit both direct and indirect actions that result in ulcer formation,” Houghton says.
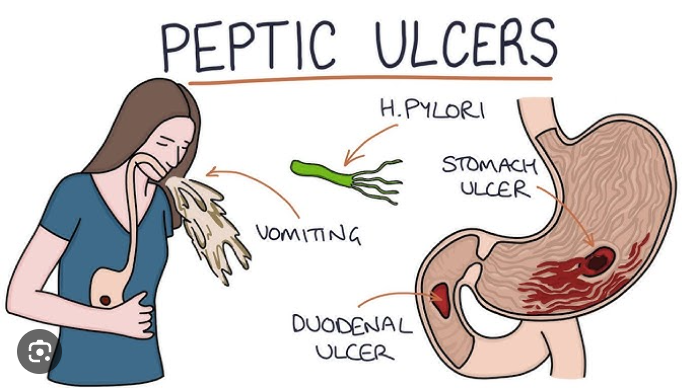
According to the Centers for Disease Control, about 30% to 40% of people in the U.S. have the H. pylori bacteria, but most of them won’t develop a peptic ulcer as a result. (The percentage of people who have H. pylori in other countries is even higher.) But in some cases, the bacterium causes inflammation of the stomach’s inner layer, leading to an ulcer.
There are several ways that you can get H. pylori:
- You live with someone who has it.
- You live with many other people, which raises your chance of exposure to it.
- You’re eating food prepared in an unsanitary area.
- You’ve had contaminated water.
- You’ve traveled to or have lived in a developing country where crowded living or unsanitary food preparation are more common.
The second cause of a peptic ulcer is the overuse of non-steroidal anti-inflammatory drugs, or NSAIDs. Some common NSAIDs include:
- Aspirin.
- Diclofenac.
- Ibuprofen.
- Naproxen.
Sometimes, there are NSAIDs present in combination medications, such as the medicines you may use for a cold. Although acetaminophen is a common pain reliever, it’s not an NSAID. NSAIDs can weaken the lining of the upper GI tract, says Dr. Ashkan Farhadi, a gastroenterologist at MemorialCare Orange Coast Medical Center and director of MemorialCare Medical Group’s Digestive Disease Center in Fountain Valley, California. If you use NSAIDs too often, even a normal amount of acid in your stomach can create the damage that causes ulcers, he explains.
Mental or emotional stress is not a cause of a peptic ulcer. This is a common misbelief, Farhadi says. Peptic ulcers are also not caused by spicy foods, although spicy foods may irritate an existing ulcer.
Risk factors of peptic ulcers
Aside from the obvious risk factors—having an H. pylori infection or using NSAIDs excessively—there are a few other factors that may put you at a higher risk of developing a peptic ulcer. These factors don’t cause a peptic ulcer, but they make it more likely that an ulcer could develop:
- Smoking.
- Drinking too much alcohol.
- Being older.
There are also certain medications, in addition to NSAIDs, that have been shown to increase the risk of developing a peptic ulcer, Houghton says. If you use these medications and use NSAIDs, you can increase your risk. These medications include:
- Selective serotonin reuptake inhibitors, or SSRIs,
- Prednisone.
- Risedronate, also known as Actonel
- Alendronate, also known under the brand name Fosamax,.
Symptoms of peptic ulcers
Sometimes, a person with peptic ulcers has no symptoms. Others have no symptoms initially and then develop severe symptoms, such as a hole in the gut or GI bleeding, Farhadi says.
You may not always know if a peptic ulcer has caused bleeding, but your body will tell you in other ways, such as by throwing up red blood or coffee-ground material, Houghton says. Or the bleeding may cause black, tarry stools.
Symptoms of a peptic ulcer can include the following:
- Abdominal pain that may be worse at night “A deep ulcer can penetrate through the abdominal wall and can actually cause a hole in the stomach, which will cause severe belly pain,” says gastroenterologist Dr. Harish K. Gagneja of Austin Gastroenterology in Austin, Texas.
- Black, tarry stools.
- Bloating or a feeling of fullness.
- A feeling of relief after you eat. However, others with a peptic ulcer actually feel worse after they eat, Farhadi says.
- GI bleeding.
- Indigestion. You may hear a doctor call this dyspepsia.
- Loss of appetite.
- Nausea.
- Vomiting up blood or black material that Houghton says is commonly called “coffee grounds.”
You also may just not feel well in general, says Dr. Tarek Hassanein, a gastroenterologist and liver specialist and head of the Southern California GI & Liver Centers, with various locations.
A slow loss of blood from an ulcer can also lead to anemia. The symptoms of anemia include:
- Fatigue.
- Feeling short of breath easily.
- Appearing very pale.
If you have a quick loss of blood, you may feel as if you’re going to pass out. If you think you’re experiencing rapid blood loss, then go to an emergency room.
Diagnosis of peptic ulcers
To help diagnose a peptic ulcer, your doctor will first ask about your symptoms. The symptoms associated with peptic ulcers could also indicate a different medical problem, which is why other testing is needed.
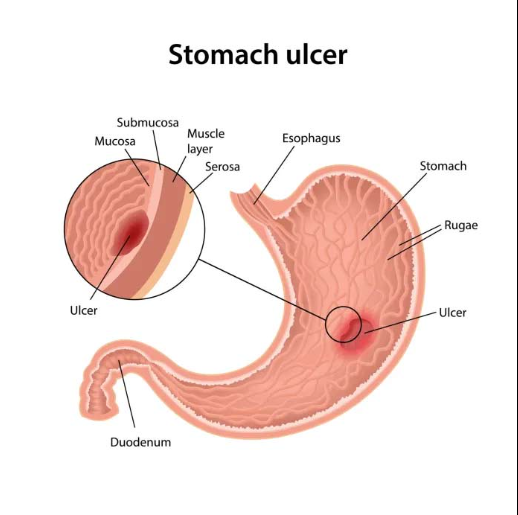
A procedure called an upper endoscopy is the most common way to detect an ulcer, according to the American College of Gastroenterology. Also called esophagogastroduodenoscopy, or EGD, this procedure involves inserting a camera with a light on a flexible tube into your mouth and looking in the stomach and small bowel.
“An ulcer is readily evident on an EGD and appears as a carved-out area in the stomach or duodenum. It may be actively bleeding as well,” Houghton says. During diagnosis, your doctor may be able to help treat a bleeding ulcer by injecting medicine or using other techniques.
Your doctor may take pictures of any ulcers or take a tissue sample for a biopsy. Gagneja says, “A biopsy may be necessary when it is difficult to distinguish between malignant (cancerous) and benign ulcers.” You may need to have an EGD done again after you’ve received treatment for a peptic ulcer.
Treatment of peptic ulcers
Finding the cause of peptic ulcers is the first step in treating them.
You will be prescribed antibiotics to aid in the removal of the H. pylori infection if it is the root cause of your peptic ulcer. Getting rid of an H. pylori infection can be challenging. Hassanein suggests that you take your antibiotics for the entire prescribed duration.
It’s also possible that you’ll be prescribed an H2 blocker or proton pump inhibitor, which are medications that lower acid. These medications go by several generic names, including ranitidine, nizatidine, cimetidine, and famotidine for H2 blockers and esomeprazole, omeprazole, and lansoprazole for proton pump inhibitors. “These drugs are over-the-counter and will temporarily lower stomach acid so the GI tract can heal,” says Hassanein.
Also read-GERD : A Patient’s Guide To GERD And Its Symptoms
images source: Google
Disclaimer: The opinions and suggestions expressed in this article are solely those of the individual analysts. These are not the opinions of HNN. For more, please consult with your doctor.