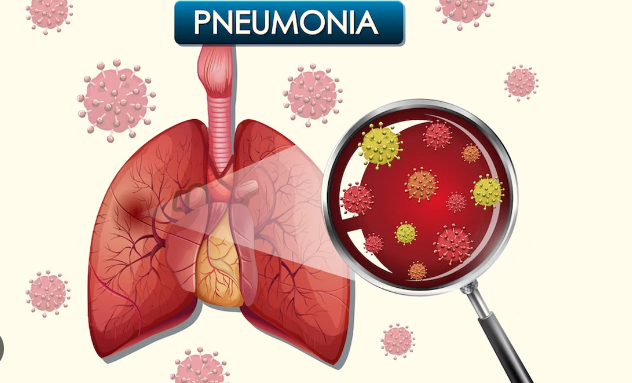
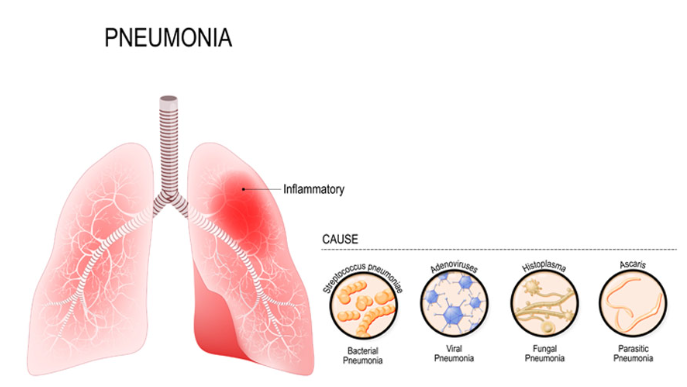
Pneumonia can be caused by bacteria or viruses, affecting treatment choices.
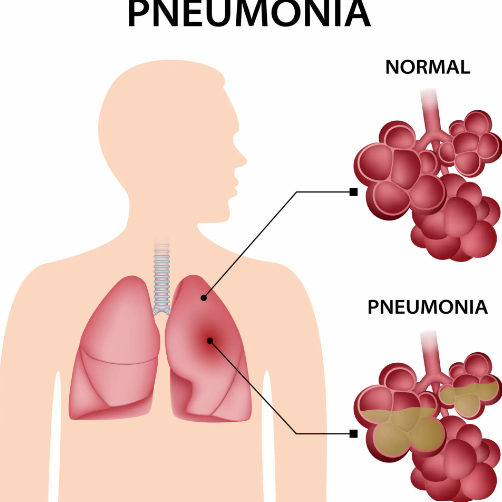
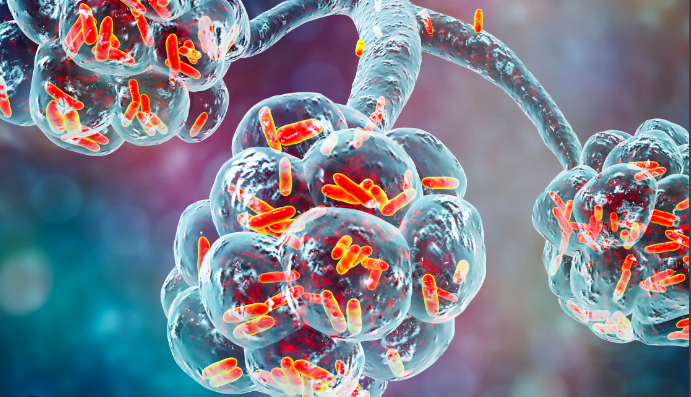
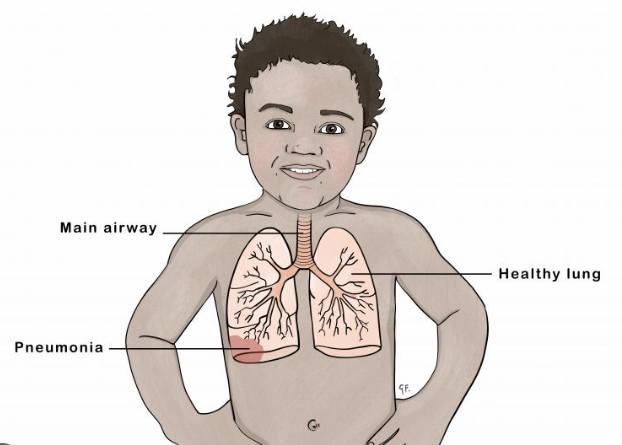
Pneumonia, an infection of one or both of your lungs, can leave you coughing, feverish, and miserable at home. And sometimes, it can land you in the hospital, struggling to breathe. It affects the air sacs of the lungs, or the alveoli. As these air sacs become inflamed and infected, they fill with fluid, making breathing more difficult and reducing the flow of oxygen throughout your body.
From relatively mild to dangerously severe, cases vary. Extremes in age are a major risk factor for it, with the most vulnerable populations being the elderly and children under five. A case of it may be fatal. Per the Centers for Disease Control and Prevention, it causes hospital admissions for approximately one million Americans each year. About 50,000 people die from it each year, and the majority of them are elderly.
Also read-Emphysema : A Patient’s Guide To Emphysema And Its Symptoms
Types of Pneumonia
A variety of bacteria, viruses, and fungi cause different types of it. These germs enter the respiratory tract through your mouth or nose. There are several ways you can become infected: If an infected person coughs or sneezes on you, if you breathe in the germs, or if you touch a contaminated surface and then touch your face, you can get it.

Causes
The following are the main categories of organisms that cause it:
Bacterial Pneumonia
Bacterial includes these types:
- Pneumococcal. This common type of bacterial pneumonia is caused by Streptococcus pneumoniae.
- Staph . Staph pneumoniosis is caused by Staphylococcus aureus. MRSA is an antibiotic-resistant form of S. aureus bacteria.
- H. influenzae. Although similar-sounding, Haemophilus influenzae bacteria are not related to the flu virus.
- Gram-negative . This is pneumonia caused by bacteria such as E. coli, Klebsiella, or Pseudomonas. (They’re called gram-negative because of how they respond to a chemical staining process in the lab.) This type of pneumonia is more common in health care facilities than in the community.
Viral Pneumonia
Viral pneumonia includes these types:
- Influenza pneumonia caused by influenza (flu) viruses A and B.
- RSV pneumonia (respiratory syncytial virus). RSV is more common in children.
- Adenoviruses, rhinoviruses and human metapneumovirus are less common causes of viral pneumonia.
Walking Pneumonia
Mycoplasma pneumonia is also called atypical or walking pneumonia. Although caused by bacteria called Mycoplasma pneumoniae, it’s milder than typical bacterial.
Fungal Pneumonia
It can develop from diseases that are caused by breathing in airborne fungal spores. Fungal infections are less common than viral or bacterial types.
In addition to contagion from outside sources, your nose can be “colonized” with bacteria without you realizing it. That bacteria may stay there indefinitely or become invasive and actually cause infection, Washer explains.

Symptoms
It can be hard to tell whether the symptoms you’re experiencing are due to a common cold or not and if you need to be seen by a doctor. The time frame provides a clue, says Dr. Heather Alden, a family medicine physician at Intermountain Healthcare in Salt Lake City.
“Most patients start getting concerned when they have an illness, like a cold, that’s lasting much longer than they expect,” Alden says. “A lot of patients come in and say, ‘It’s been almost two weeks and I’m still having fevers.’ So it’s the length of symptoms—the persistence of fever or new symptoms. They’re having chills; they’re coughing more mucus and thick phlegm. These are usually reasons why people eventually come into the office.”
These can be its symptoms:
- Cough that persists.
- Purulent cough with greenish/yellow phlegm.
- Blood-tinged phlegm.
- Fever and chills.
- Wheezing.
- Breathing difficulty.
- Night sweats.
- Nasal flaring and rapid breathing in infants.
- Chest pains.
- General malaise or decreased energy.
- Appetite loss.
Diagnosis
Even with milder symptoms, such as a low-grade fever, an ongoing cough, feeling tired, or loss of appetite, you might need an examination from your primary care provider. “I usually tell patients: If you’ve been having cold symptoms for seven to 10 days and things still aren’t getting better, that’s when you should go see your doctor,” Alden says.

To diagnose it, health care providers evaluate your symptoms, listen to your lungs with a stethoscope and possibly order a chest X-ray or other imaging tests. The extent of testing varies depending on whether your infection is likely community-acquired or hospital-based, your age and medical history and the severity of your symptoms.
.
Patients admitted to the hospital typically get blood work done and sometimes have sputum samples taken to isolate the particular bacteria causing it, LaFon says.
Treatment
Treatment at home typically involves oral medication and supportive measures.
- Antibiotics
- Antivirals
- Supportive Care
- Complications

Also read-Knee Pain : A Patient’s Guide To Knee Pain And Its Symptoms
images source: Google
Disclaimer: The opinions and suggestions expressed in this article are solely those of the individual analysts. These are not the opinions of HNN. For more, please consult with your doctor