The chronic condition can be debilitating, but treatments are expanding and improving ulcerative colitis.
After using the restroom, Jordan Wilson noticed blood in the toilet and chose to do nothing, as would be expected of most stubborn 26-year-old men. However, Wilson was forced to confront the beet-red issue when, several months later, he discovered that there was more blood in the toilet than water. He hauled himself to his primary care physician after he started having cramps and stomach pain.
Following Wilson’s doctor’s ruling out a bacterial infection (antibiotics proved ineffective), the gastroenterologist suggested a colonoscopy. Wilson was diagnosed with ulcerative colitis after the procedure.
Also read-Irritable Bowel Syndrome : A Patient’s Guide To Irritable Bowel Syndrome And Its Symptoms
What is ulcerative colitis?
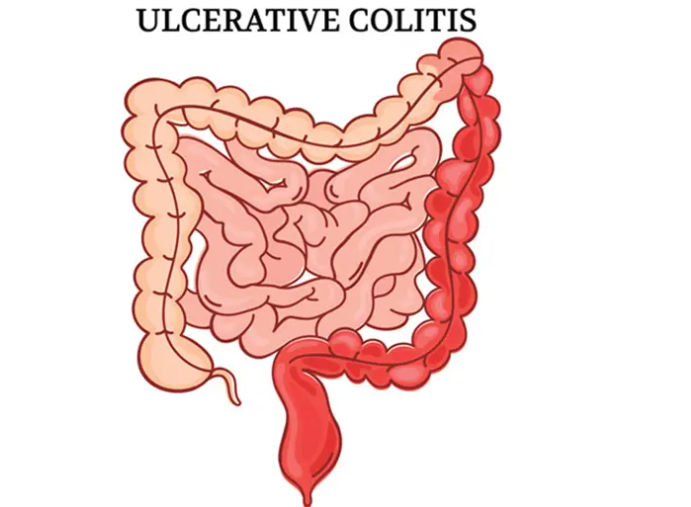
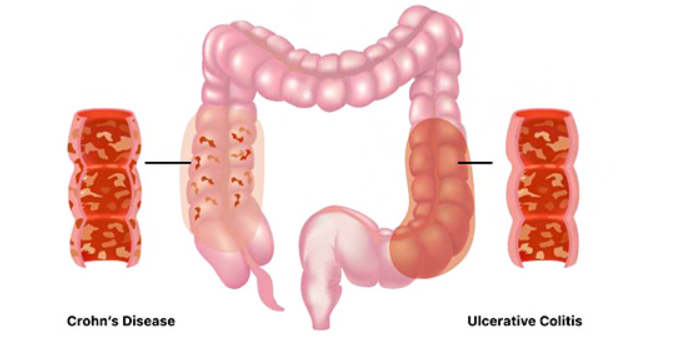
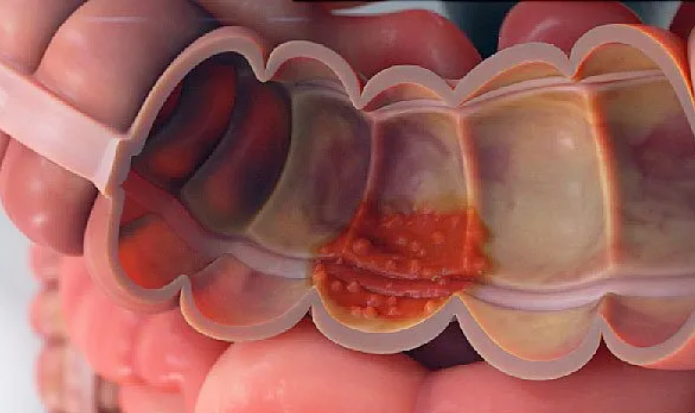
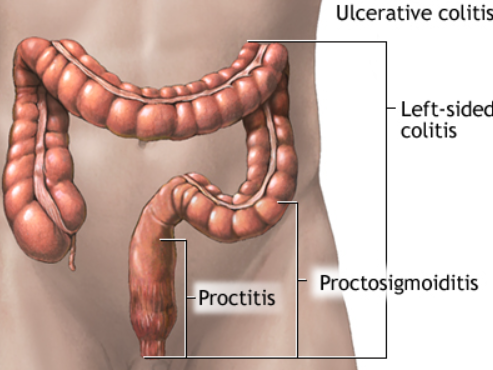
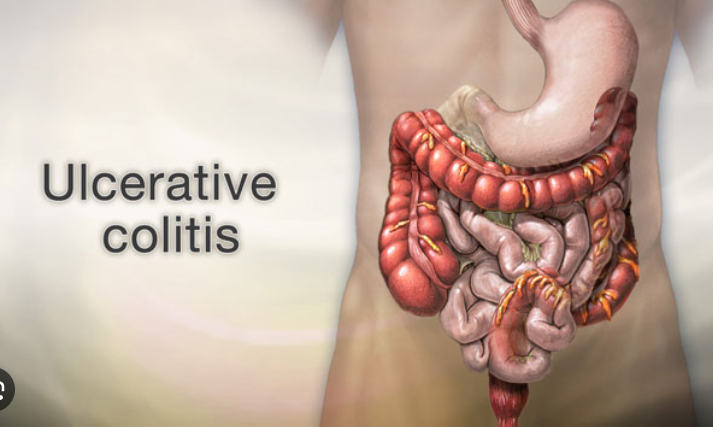
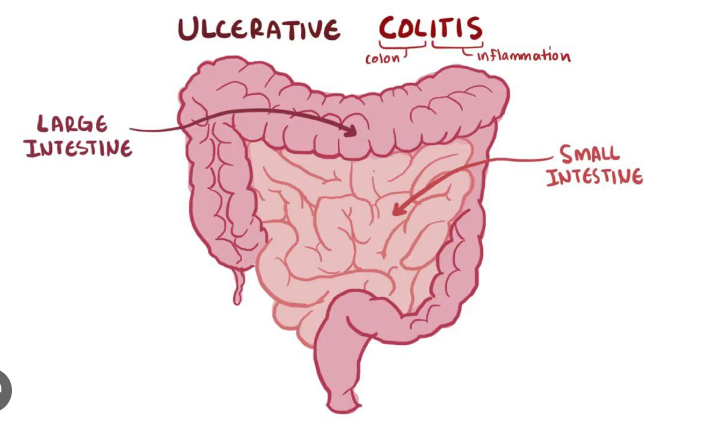
The large intestine (also referred to as the colon) is impacted by the chronic autoimmune disease ulcerative colitis. The ailment, which is categorized as “inflammatory bowel disease” or IBD along with Crohn’s disease, results in the colon’s lining becoming inflamed and developing ulcers. These sores can cause stomach pain, bleeding, and the need for up to 20 daily bowel movements.
Dr. David Rubin, a medical professor and head of the University of Chicago Medical Center’s gastroenterology, hepatology, and nutrition section, compares it to “food poisoning that doesn’t go away.”
A healthy rectum, which is the final six inches of the large intestine, “stretches, stores, squeezes, and senses,” but an ulcerative colitis patient’s rectum does not. “It can’t sense to know when you need to pass gas or something else; it doesn’t stretch properly, and it cramps and can cause immense pressure on the bottom,” says Rubin. “People take their rectum for granted until it doesn’t work.”
Causes
Although the precise cause of ulcerative colitis remains unknown, scientists and medical professionals are aware that, similar to other immune disorders, UC is influenced by genetics, the immune system, and environmental factors. The Crohn’s and Colitis Foundation of America states that “foreign substances (antigens) in the environment may be the direct cause of the inflammation, or they may stimulate the body’s defenses to produce an inflammation that continues without control.”
Many factors, including the following, are assumed to interact to cause ulcerative colitis:
- Autoimmune response.
- DNA.
- Diet heavy in fat.
- Environmental elements, like a virus or antibiotics.
In addition, certain foods and stress may trigger flare-ups.
In general, ulcerative colitis tends to affect men and women about equally, but U.S. studies suggest it’s more common in men, according to the CCFA. You can have ulcerative colitis at any age, but it often occurs between the ages of 15 and 30 years, or later in life, from the ages of 50 to 70 years. It’s more common among whites and those of Jewish descent.
Symptoms
While symptoms and their severity vary among people and with each “flare-up,” or period with symptoms, they can include:
- Rectal bleeding.
- Rectal pain.
- Urge for bowel movements (even when nothing is produced).
- Diarrhea.
- Bloody stools.
- Abdominal cramps.
- Fever.
- Pain (usually on the left side of the abdomen)
- Unintended weight loss.
- Fatigue.
- Dehydration.
- Joint pain.
- Mouth sores, nausea, and vomiting
- Skin lumps or ulcers
- Anemia.
Diagnosis
To confirm a case of ulcerative colitis, a gastroenterologist will likely perform a variety of tests, such as:
- Blood work to detect infection, markers of inflammation, and anemia.
- A stool culture to test for pathogens.
- A fecal blood test to indicate whether there is bleeding in the intestines.
- A colonoscopy will provide a clear view of your colon. During the procedure, your doctor may take small samples of tissue (a biopsy) for laboratory analysis.
- An abdominal X-ray to assess the extent of the disease.
Treatment
The good news is that ulcerative colitis is manageable, and treatment options are expanding and improving. Not only can they help people feel better, but increasingly, they promise to actually help repair the lining of the colon. “The goal of managing colitis is remission, which means feeling perfect,” Rubin says. “No blood, no urgency, sleeping through the night without bowel movements, and able to pass gas without fear of leaking.”
To achieve that, medical treatments target inflammation. “The future is exciting because we’re figuring out different immune mechanisms of inflammation, and there’s a large interest in drug development in this field,” says Dubinsky, who is also chief of pediatric gastroenterology and nutrition at Mount Sinai’s Icahn School of Medicine.
There are four main types of drugs that are used to treat the inflammation from ulcerative colitis:
- Aminosalicylates, which limit digestive tract inflammation,
- Corticosteroids (aka “steroids”), which can suppress the immune system in the short term
- Immunomodulators, which work to calm your immune system over the long term,
- Biologics,which interrupt inflammation-causing pathways.
In some cases, people with colitis undergo surgery to remove the colon and reconnect the small intestine to the rectum. Wilson went this route after other treatments failed. While he still has to use the bathroom up to 10 times a day, which inevitably interrupts his work and social calendars, and he needs to drink lots of water to account for his missing colon (which absorbs water), Wilson’s life is far more “normal” than it was before. “I wouldn’t wish my ‘normal’ on anybody, but it’s a lot better than being sick,” he says.
Also read-Crohn’s Disease : A Patient’s Guide To Crohn’s Disease And Its Symptoms
images source: Google
Disclaimer: The opinions and suggestions expressed in this article are solely those of the individual analysts. These are not the opinions of HNN. For more, please consult with your doctor.